Episode Transcript
Interviewer: Someone's diagnosed with epilepsy, given medication for the seizures, and a year later still experiencing seizures. At what point do you go see a specialist?
Dr. Sindhu Richards is an expert in medically refractory epilepsy. Dr. Richards, when would somebody come and see you?
Dr. Richards: So we definitely say a year should be the general guidelines, but we try to be a little more proactive than that even. So, right now, the American Academy of Neurology has set out like a guideline saying that if a patient with epilepsy has been seen by the primary care provider and it's been three months where they're unable to treat the seizures effectively, they should be referred to some sort of neurologist, a general neurologist or an epilepsy specialist. And then, if a patient is seeing a general neurologist for a year with untreated seizures, those people should definitely be referred to an epilepsy center.
Interviewer: And after you reach that year, it's really not something that you should put off if you're still having seizures without medication. What are some of the dangers of doing that?
Dr. Richards: In terms of the biggest concern we get about uncontrolled seizures is there's a phenomenon called SUDEP, which stands for sudden unexplained death in epilepsy. And we really don't know the clear mechanism. We just know that people who have uncontrolled seizures are at higher chance of that. So that's the scariest thing we worry about for people who have uncontrolled seizures.
And then, in terms of like other complications, so people, you know, having ongoing seizures can really affect daily life. So when you're having seizures, you're unable to drive. You can't operate heavy machinery or be on heights. So it depends on your work situation as well. But the biggest one that impacts people is the driving aspect. So it can really affect your quality of life in that sense.
And then, also depending on where the seizures are coming from, most people kind of developed some memory problems in terms of ongoing seizure activity. So that's a common complication we see that we try to avoid, if we can treat them early.
Interviewer: At this point, they walk into your office. Walk me through the diagnosis process that you use to get to a diagnosis of medically refractory epilepsy. And from what I understand, one of the first things you might look at is, "Was the initial diagnosis of epilepsy correct?" Because I guess it's like 13% to 15% of people that are diagnosed with epilepsy actually have something else.
Dr. Richards: Yeah, exactly. So that's a really important step to clarify too. And one of the ways we do that is, obviously, getting a very good history in terms of what exactly they're doing from the patient. But also a really important aspect is getting a history from the bystanders because they're the ones that are seeing what the patient's actually doing.
A very common diagnosis that epilepsy can be confused with is what we call psychogenic non-epileptic spells. So some people, due to like stress or anxiety, their body can react in a way where it looks like they're having a seizure when actually they're not. Like, we look at the brain activity, it's actually completely normal during that time. So if we're uncertain about the diagnosis, that's definitely the first step to try to confirm that. And one of the ways we typically do that, that is available at epilepsy centers, is that we bring people into the hospital and monitor them on the EEG, which is the brainwave study. And we try to capture their typical episodes so that we can see exactly what's going on in the brain. And if they do have epilepsy, it helps us see where it is coming from in the brain. So that's usually the first step we do to kind of clarify the diagnosis.
And then, after that, in order to be diagnosed with medically refractory epilepsy, you have had to have an adequate trial of two anti-epileptic drugs and are continuing to have seizures. So in terms of what we mean by adequate trials is a lot of people stop medications because they have side effects from them, and so that wouldn't mean an adequate trial. So if you stop a medication because of side effects and you're still having seizures, you still have to have a good trial of two drugs before you can be considered medically refractory epilepsy.
Interviewer: So, at this point, if you do then come to the diagnosis that it is medically refractory epilepsy, what are the steps at that point?
Dr. Richards: When you see a patient who's diagnosed with epilepsy and you start a new medication, so an anti-epileptic drug, about 50% of patients will become seizure-free on that. So that's a really good amount of people who will be seizure-free. Once you get to the second drug, an additional 13% will be seizure-free.
So then you're kind of left in this third category of patients who are not seizure-free on medications. And you usually tend to try different trials, but they continue to have seizures. So it's that third of patients who are diagnosed with epilepsy that are considered the medically refractory.
And so, you know, like I said, the main concern for these people are the long-term side effects of having seizures, the risk of sudden death. So we really try to offer other options. And one of the biggest options we have to offer is surgery. And so there's a lot of workup to be done before we consider surgery because, you know, that is a very big step and it's a big deal for us and for patients too to go through potential brain surgery.
So the very first step, in terms of treatment of medically refractory epilepsy, is bringing someone into the hospital where we try to capture their seizures. Because, in order to see what surgical options a patient has, we need to know where the seizures are likely coming from. And so what we'll do is we'll bring the patient in, we'll stop all of their anti-epileptic drugs because we want them to have a seizure when they're in the hospital. And then, once we've gotten about two to three seizures and they're reliably from the same location or let's say they show us that the patient has seizures coming from several different locations, we'll know what the next step could be. So that would be the very first step.
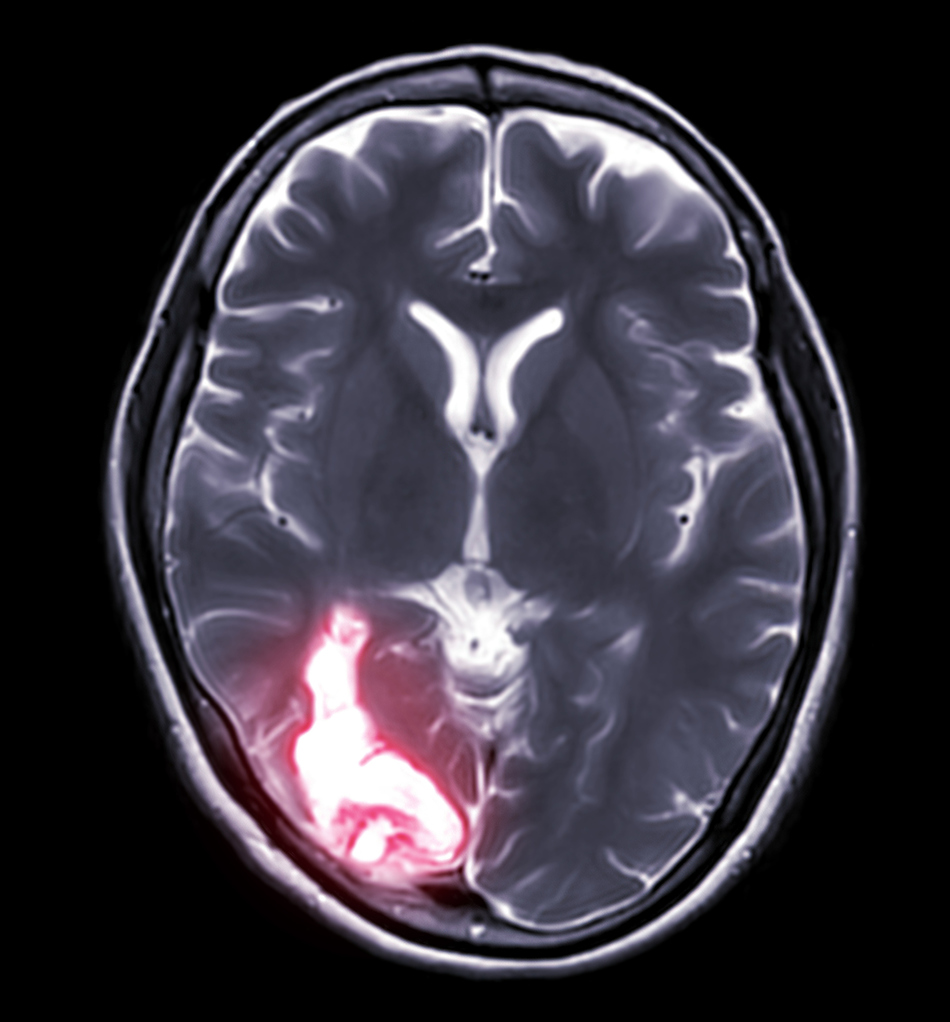
And then, after that, we typically try to do some non-invasive evaluations to help us pinpoint even more where the seizures are coming from. So this includes different type of imaging. So patients will definitely get an MRI because we try to see if there's a reason or a lesion or a structural cause as to why they are having seizures.
And then we'll also do some more advanced imaging. So we'll do what we call a PET scan, which is a nuclear scan. So we inject dye and we look at the areas of activity in the brain. And usually, in patients with seizure, the activity of the brain is decreased in their seizure focus. So that helps us kind of guide us towards where we think the seizures are coming from as well.
And then we'll typically send them to a neuropsychologist. And the neuropsychologist will look at their memory, their language, and other important functions of the brain so we can figure out where these important functions are and to make sure that they aren't affected when we consider surgery.
And then, lastly, to kind of do that as well, we do what we call functional MRI, where we ask them to do some different language tasks and some different motor tasks because then we can see exactly where in the brain it lights up and we know where those tests are coming from so we avoid those areas in surgery as well. So there's quite an extensive workup to do before you even consider the surgical options for a patient.
Interviewer: And after you do all of these tests, you have a much better idea then of what you're dealing with, where the surgery needs to focus on. At that point, is the type of surgery that the patient will get really based on what those tests indicated, or are there some choices the patient will have to make in surgical procedures?
Dr. Richards: Yeah. So there are definitely choices that we can make, whether like how invasive the patient is willing to go versus like if they want to be a little more conservative, because we have options where we can actually take out the brain. But we also have a lot of neuromodulation, which are devices which wouldn't require any major, you know, removing of the skull in terms of brain surgery and things like that. So it's a ongoing discussion with the patient about what we think would be the benefits versus risks and what they feel like would be an acceptable surgery and things like that.
So after those initial testings are done, we'll typically put EEG electrodes directly into the brain. So it's a minor surgery, where we drill a hole in the skull and we put electrodes right into the brain. And so that gives us an even more precise localization of where the seizures are coming from. So that's typically a step we will do even before we consider surgery.
Interviewer: And you mentioned some of these outcomes are like a 50% reduction. Generally, what is the reduction in seizures that a surgical procedure can offer? And then, you know, if there still are seizures, how are those addressed going forward in the future if, you know, an individual is resistant to medication, is not able to control it with medications?
Dr. Richards: Yeah. So this is why we like to get to people early because the data has shown . . . so let's say you have a patient with medically refractory epilepsy and you continue to try to treat them with different medicines. Only about 8% of those people will become seizure-free. Versus with surgery, about like 65% may become seizure-free. So that's a great difference in terms of seizure freedom. And you can even imagine, if people don't become seizure-free, they'll at least have a significant seizure reduction.
So the big thing to know is that people who go through epilepsy surgery, it's not an alternative for medicines. So these people will, generally, remain on medicines to make sure that we control the seizures. It just means that they might be on less medicine, which is great because medicines can cause side effects, it might not need as much. So that's an important thing to clarify for people because people think they can just get surgery and come off everything. But we do have to keep people on medicines to give them the highest chance of seizure freedom.
Interviewer: And I'd imagine it varies from all the different types of surgeries because, you know, you mentioned some actually require the skull to be open, which I even have a hard time even saying. That sounds a little scary. And then there's some of the more non-invasive procedures. What type of recovery could a patient look at after receiving surgery?
Dr. Richards: Yeah. So for the invasive ones, where you have like either . . . the invasive one is really like the lobectomy. And for that one, I would say, you know, in terms of like people who are in the hospital, they're only in the hospital for a few days, but usually it takes like about a month, I'd say, to fully recover from that surgery. In terms of for the neuromodulation procedures, the patients usually go home the next day and there really isn't that much of a significant recovery, people do really well.
Interviewer: I don't know if a question is going to come out of this or not, but listening to you talk about just the process of diagnosis and then the process of treatment, just how incredible is all of it that we can do any of it, right? That you have the equipment and the expertise and the training to be able to go in and pinpoint where this problem might be in the brain and then be able to go in and do something about that. I mean does that resonate with you on any level whatsoever or is it just something you do at this point?
Dr. Richards: Yeah. So that's why I fell in love with epilepsy. You know, going through neurology residency, we do deal with a lot of different devastating conditions. But for epilepsy, I really felt like there was something we could do and something we could offer. And the surgical options for epilepsy is really what brought me into this field because I felt that it was just amazing that what we could do and the different devices, and I think we're continuing to kind of develop more and more things that are going to be on the horizon. Like, 10 years ago, it wouldn't have been an option for this patient to have gotten that surgery and she still would have been having seizures. So I'm continuing to be hopeful that, down the line, we're going to have a lot more options, especially for our generalized patients because these people don't have a lot of surgical options at this point.