Episode Transcript
Announcer: Examining the latest research and telling you about the latest breakthroughs, the Science and Research Show is on The Scope.
Interviewer: Ebola outbreaks have increased in frequency in recent years, culminating in the alarming epidemic that we face today. My guests, Dr. Michael Kay, professor of biochemistry at the University of Utah, and Dr. Debra Eckert have reported in the journal "Protein Science" a universal drug target against Ebola that could prevent future outbreaks.
You found a drug target for potential treatments against Ebola. What advantage does your target have over others that are being developed that you know of?
Dr. Eckert: What we did is we're looking at a particular area on the protein on the surface of the virus that's conserved across all known strains and species of the virus. Our drug target should be able to be used in screens to identify drugs that will be able to combat any Ebola virus outbreak. The virus in the current outbreak would be susceptible to such drugs, and future outbreaks, even if it was a different species.
Interviewer: I'm going to ask the question that's on everyone's mind. Is it possible that your new research finding can help in the current Ebola crisis?
Dr. Kay: We're focused on the long term, and the likelihood that this outbreak will not be unique and that this is going to be an ongoing problem in the future. Given how slow drug development processes are, developing from a target to a treatment that's available just takes too much time to be of real value in the current outbreak.
We're taking a long term view to have one agent that could be stockpiled and ready to go for diverse Ebola strains, versus having to stockpile a large number of individual distinct therapies for each of the different strains that are out there. We think this is something that will be more workable long term, more economical, and allow more rapid access for people who need the drug in an emerging epidemic without having to identify exactly which strain is involved.
Interviewer: Is there an impetus for creating a universal drug target as you've done? Do we know anything about how quickly the Ebola virus mutates?
Dr. Kay: The current outbreak has given us a tremendous amount of information on this that we haven't had before, because there haven't been that many who had Ebola before. The early data is that the virus mutates at a somewhat surprisingly high rate. The virus is changing during this current outbreak.
Dr. Eckert: It's important to note that we've looked at that sequence data that is available and our region has not changed in the current outbreak.
Interviewer: What are the next steps toward creating a treatment that utilizes this target?
Dr. Eckert: The next step is to use this target to screen for inhibitors that would stop Ebola from entering cells. We have started the screens in collaboration with our development partner, Navigen. We do have some preliminary results. Also, we would invite the scientific community to use this drug target to screen other types of molecules. Essentially, anything that was identified in the screen with this universal target should be effective against a broad range of Ebola virus species.
Interviewer: What do you think the hypothetical time scale could be moving from the screens to an actual treatment?
Dr. Kay: With Ebola, you can't do clinical trials in the traditional sense. You can't have, for instance, a group of patients that get placebo or the drug. The virus is not so common, so finding patients who have it at any given time may be difficult.
There's an alternate process for these kinds of very severe diseases that you can't do a traditional clinical trial. It's called the animal rule. The idea is that you can prove the drug is safe and then use an animal model to show that it works well in whatever model best mimics the human situation. That's all you can do. Then, you have to use it in the field in a crisis.
In theory, it could only take something more like three years, rather than the traditional ten.
Interviewer: Maybe we should back up a second and talk about what is this mechanism that you're targeting.
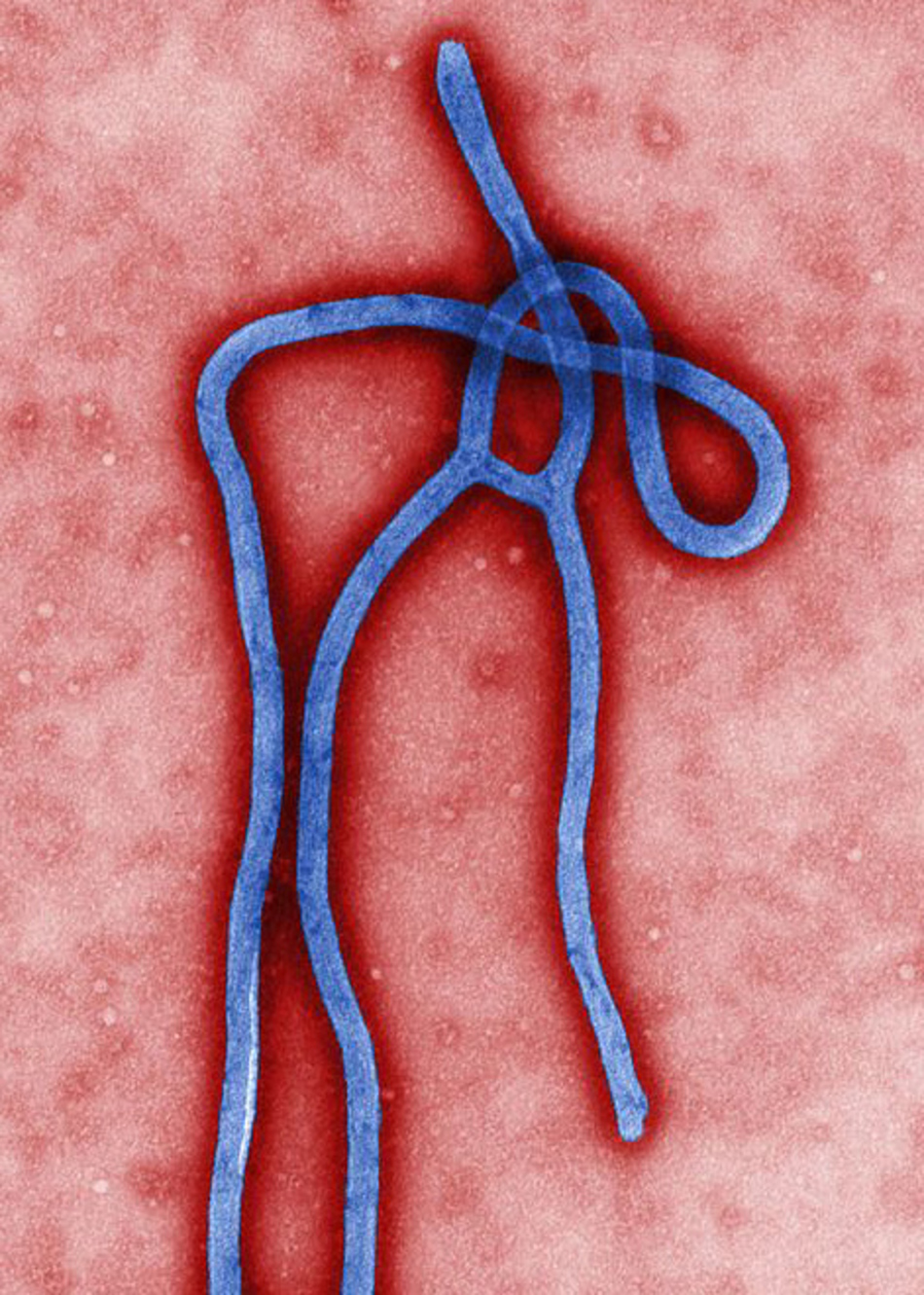
Dr. Kay: The region that we've identified we call the N-trimer. It is a trimeric coiled coil, three helical segments that bind together that play a very important role in Ebola's ability to enter and fuse with cells and to deliver its genome to the cell. That's the process that's the early part of the virus life cycle and what we're trying to stop to prevent the virus from ever getting into the cell. This machinery is extremely highly conserved. Importantly, it can be made separately from the rest of the virus and therefore is very convenient to use as a drug target.
Interviewer: Do you know the state of other treatments that are in development right now?
Dr. Kay: There are a number of treatments that are at the latest stage of development that are being talked about in the context of the current outbreak. The most important one that's been talked about is a cocktail of monoclonal antibodies, and this is called ZMapp. You may have heard about this in the news. Several patients were treated with this drug as a compassionate use in the current outbreak. It's such a small number of patients it's very difficult to tell whether or not that antibody cocktail has been successful or not.
There's been some very impressive data in monkeys showing that this drug works extraordinarily well even given at very late stages when the animals are already significantly symptomatic. That kind of data creates a lot of excitement in the field that this approach is likely to be successful in humans.
Unfortunately, there's a supply crunch right now. Antibodies are difficult and expensive to make. It takes a long time to build up a supply. This company has completely run out of antibody and is racing to make more in hopes of being involved in this current outbreak.
It's worth pointing out as promising as that therapy is it's focused on just one strain of Ebola, so it's not expected to work on other strains.
Interviewer: What are your next steps?
Dr. Kay: Now that we have this target in hand and we've validated its use, we are well underway in screening for mirror image D-peptides against this target. Our next stages are to optimize the promising hits that we already have, then work with our collaborators who have the ability to work with live Ebola, something that we can not do.
In particular, the U.S. Army has a wonderful infectious disease lab called USAMRID. We would send samples to them for testing in either cell based assays, which are relatively simple to do, to see if we can keep Ebola out of a cell, then ultimately animal based assays. They have a specialized lab for working with live Ebola, and that's the definitive testing to see if this is effective before advancing to human trials.
Announcer: Interesting, informative, and all in the name of better health. This is The Scope Health Sciences Radio.