
Host
Heather Simonsen, MA
Public Affairs Manager
Guests
PJ DiPentino
Bladder cancer patient at Huntsman Cancer Institute
Lexi DiPentino
Caregiver
Amelia Thelin
Patient Navigator
Episode Transcript
Topics by Timestamp
- Welcome and Introductions (00:51)
- PJ and Lexi’s Story (03:18)
- Traveling for cancer care in another state (06:33)
- Finding a place to stay during treatment (07:34)
- Patient Navigation Experience (10:07)
- Health Update (16:26)
- What does a cancer-free frontier look like to you? (21:13)
- Welcome, Amelia Thelin, Patient Navigator (22:49)
- Challenges of patients who live far from NCI-designated Comprehensive Cancer Center (25:35)
- Relationships with patients (28:20)
- What needs to be done to treat patients in their own home towns? (31:14)
- Most rewarding about being a patient navigator (33:11)
- What does a cancer-free frontier mean to you? (34:20)
- End Credits (35:29)
Welcome and Introductions (00:51)
Heather Simonsen: Hello and welcome to a Cancer-Free Frontier podcast, where we ask the question, can we create a cancer-free frontier? I'm your host, Heather Simonson.
I'm so glad you're all here with us today. We're talking about the long road to treatment. A cancer diagnosis can turn your life upside down and then having to uproot and travel long distances for surgery and treatment. I can't imagine but it can make it even tougher. And our first guest knows that struggle all too well. I'd like to introduce PJ DiPentino and his wife Lexi, who are joining us from Livingston, Montana. Hello, and welcome.
PJ and Lexi DiPentino: Hi, good morning!
Heather Simonsen: We're so glad that you're with us today. We just love our patients. And I understand you have a really special story. But I first want to start with telling us a little bit about Livingston, it sounds like just a beautiful place.
PJ DiPentino: It is, you know, it's a hub on the northern entrance to the Yellowstone Park and located along the Yellowstone River. And it's a nice little touristy-type community that we have in Livingston and we're very fortunate that my wife owns a store located in Livingston, where we cater to Montana residents and artists.

PJ DiPentino and his wife, Lexi
Heather Simonsen: Wow, that sounds so charming.
PJ DiPentino: It is.
Heather Simonsen: And I understand you're a father and a grandfather.
PJ DiPentino: Yes, the two best jobs in the world. It's the only job I have I'd gladly get up and do every day. You know, my children, were there for this whole thing. People don't realize, when you're sick and you have cancer, it affects everybody, it doesn't just affect you as a person or your spouse, of course. The difficult conversation telling my children I was sick and them, you know, worried for me and me worrying about them worrying for me and it's just a never-ending process that affects everybody. Anything that that helps to make that easier on the situation is what you're looking for and that's exactly what we got through Huntsman.
PJ and Lexi’s Story (03:18)
Heather Simonsen: I'm so glad to hear that. And let's talk a little bit about that. I mean, life was good. You're doing well there in Livingston. And then, what happened? When did you realize hey, something's not right?
PJ DiPentino: Well, at about Christmas time I just wasn't feeling well. I was tired and had chronic headaches, just something wasn't right. I couldn't change anything by diet or vitamins. I went and saw the doctor and he just says it could be, you know, my situation was prostate and bladder related. I had a tumor in my bladder and when things started to go bad was about February when I started to notice things that made me believe I had a serious problem. We went to the emergency room and were notified at the emergency room after some testing that I had cancer. Not cancer, but I was showing a tumor in my bladder that was causing the issue. That was that was probably the most heart wrenching conversation when the physician in the emergency room said, “Hey, you need to go to your urologist.” I remember when he walked out the door, I looked at my wife and I was in disbelief. I said, “Did he just say I had cancer?” and we were just staring at each other. There's so many things and emotions that come to you when you hear that, that diagnosis. You're just like, “What is going on?” You know, “What? What?!” It took a while before we realized it, but then we went to the urologist and onto the oncologist, and onto the journey to Huntsman.
Heather Simonsen: That moment had to be so tough. I mean, we've all been there, where you're waiting, “What is going on? What's wrong?” You're waiting for a diagnosis, but you're thinking, “Oh, it's, you know, it's probably nothing.” Then to hear, like you said, to hear that word, it has to kind of stop time in that moment, and really change your life.
PJ DiPentino: It was the change. It was the change of our life, went from normal to something that we really never prepared for. We never thought that I'd be sitting here, you know, talking about this, or I'd be going through it. I think that was, that was the change in our life, It's crazy, when you are facing mortality, you start thinking about everything you did in your past and everything you want to do in your future, and this being sick is like a hurdle that’s stuck right in between that. It's, “How do I get over this to get to the other side?” That's the mindset, it was like, we got to do whatever it takes to get me healthy so I can maintain what I built and where I'm at in my life. That was our goal, we got to beat this thing one way or another, it doesn't matter what it is. But, you know, the other option is not a possibility.
Traveling for cancer care in another state (06:33)
Heather Simonsen: Absolutely. And you traveled to Huntsman Cancer Institute for your surgery. Now what is that about a seven-hour drive?
PJ DiPentino: We actually took a plane. Part of my cancer was, you know, you just had to be close to the bathrooms and it was one of those things where we decided to do. My wife handled most of that stuff because I was too ill and I'll let her attest to what we went through to get that.
Lexi DiPentino: Part of choosing to go on the plane was not only because he had frequency of urination, but on the trip home his doctor didn't want us to be out in the middle of nowhere after surgery and something happen and not be close to a hospital. Traveling by plane was the most effective and logical way to go.
Finding a place to stay during treatment (07:34)
Heather Simonsen: That makes so much sense. But what was the biggest challenge? You're far away from your kids, your friends, I mean, that had to be really tough, and here you're having major surgery.
PJ DiPentino: Yeah, it was Fourth of July weekend too, which didn't help. But I went in and I knew that we would be in Utah for two weeks minimum. One of the first weeks was in Huntsman after the surgery, and then after that, we found a facility that was able to house us: The Hope Lodge, located in Salt Lake. The Hope Lodge was for people who are going through cancer and they're fighting that battle, the American Cancer Society sponsored it. We were given a room at the Hope Lodge with a little living room area and a bedroom area with two beds, and then there was a communal kitchen area on the main level where all the residents had their own little kitchen locations. You know, I've got to heal with other people who were fighting the same battle and that was just an incredible thing for me, was to be able to be around other people who were in similar situations but have the dignity and decency to have our own space.
Lexi DiPentino: And that was very huge for us. We were there before and after his surgery. I did not know about that facility until I was connected with folks at the Huntsman Center, so we're very grateful for that.
Heather Simonsen: That’s wonderful to hear.
PJ DiPentino: That’s part of the challenge. You know, the challenge is not the 600 miles to get here, but how do you recuperate? How do you heal and all that while being without? You know, without my children, without my support, without my family, just my poor wife who was through thick and thin. Oh, one of my sons did fly to Utah for last couple of days to help me get ready to come home and he was the first child I had seen in, going on three weeks, so that was really tough. You’re kind of out by yourself but we surrounded ourselves with positive people and positive situations. Part of that was with the help that Amelia brought to us while we were going through that process.
Patient Navigation Experience (10:07)
Heather Simonsen: Yes, let's talk about, you mentioned Amelia, your patient navigator. The health care system, let's face it, it is not easy. I mean, it is a tough process. How did Amelia help you?
PJ DiPentino: I can't, you know, it's hard to put into words. When you're struggling, you're in an area where you don't know anybody, and just everything is tough, and Amelia was amazing. When we checked in, we saw her right away. You know, you get there on a Friday and you're having surgery on Monday, so there's a lot of stress and worrying. She was so kind, I mean, she showed up with tickets to the art festival that was going on downtown, and what a blessing that was. As we walked through town together and just enjoyed everything about Utah and the people. It was really, really nice.
Lexi DiPentino: And she helped us even before we stepped in to Salt Lake, you know, she was my contact there. From the very beginning, life is very hard as a caretaker. I'm running our store, I have a full-time job also on top of that, and then trying to pick up everything that my husband did at the house, there were a lot of roles that I was playing. I wasn't always on the ball with everything and Amelia even reached back out to me like, “Hey, how are you doing?” Just to check in on me and I was like, “Oh my gosh, I still have to book a hotel,” or I have to do this or whatever. It was really nice. From the very beginning, she was there to help figure out what type of travel we needed, how there are different flight opportunities and stuff. She just gave me everything that I needed or opportunities I could potentially use to travel and then allowed me to kind of figure out how it worked best for us. And she was always there, oh my gosh, I can't even explain how amazing she was through the whole process.
Heather Simonsen: We actually have Amelia in the studio today and we're going to be talking to her in a minute. But I'm just so touched hearing you explain how much she helped you. I can tell you, she is touched. It's not very often that you hear how your job really impacts someone's life in such a powerful way.
Lexi DiPentino: I'm crying right now just thinking about all the help she gave us. She was just such a blessing. We could not have done it without her.
PJ DiPentino: Yeah, it was really comforting. Like I said, you have so much to worry about and you’re thinking about and you're stressing out, and then the fear of the surgery, you know, we're both scared to death. We're wandering around a town where we don't know anybody we're not even sure what's ahead of us, our children aren't here, our people to lean on, and she stepped right into that role for us. I mean, she really was able be there for us. To me the epitome of the word support is that she was support, she was support from so many different ways, so many different things that made it a worthwhile decision. We could have went to Denver, we could have stayed in Montana, we chose Huntsman because of the facilities, the type of cancer I had, and the treatment that I thought I could get made taking this big risk of going all the way across country to get this done worth it. I sit here today attesting that I'm not cancer free, but I am better off than I've ever been in a long time and that experience is what brought me here.
Heather Simonsen: It’s almost like a substitute family member, a stand in if you will. Is that how you describe it?
Lexi DiPentino: Absolutely, I would explain it that way. Somebody who just steps in, is right there by you whenever you need. We decided at the last minute when our son was coming that we wanted to rent a car so we could drive around because we didn't know what it was going to be like until we got there. I reached out to Amelia and she right away was able to get us gas cards which was just amazing. We were able to go and drive around with our son a little and do some sightseeing when he was with us before PJ’s last doctor's appointment and before we left. It was just very nice.
PJ DiPentino: You know, one of the things too is, by my son being able to come in the end, my wife was worn out. At that point we'd been three weeks into this, she was tired, worn out, had been just beat up. Just the fact that my son was there and was able to take mom and the two of them got lost for about six hours in Salt Lake with each other, was so much therapy for her and for me. Those small little things that help us to be able to do that was what created the positive experience. I couldn't imagine, I told my wife at one point, I couldn't imagine going through this battle by yourself, without your family, without the support. I never, as a single man, would have figured out Amelia even existed. I wouldn't have known what was available, I would have just toughed it through and who knows if I even would have made it. Just that positive experience having that local contact, having somebody that came to check on me after the surgery, that was really cool. My wife, I don’t remember it, but she said, “Amelia came by and wanted just to see how you were doing.” I mean, that's the personal touch that made a world of difference because that's what you would do, you would check on a family member, you checked on a loved one to make sure they're okay.
Health Update (16:26)
Heather Simonsen: Well, I really appreciate you sharing that PJ and Lexi. It's so good to talk to you today. What can you tell us about your condition now? How are you?
PJ DiPentino: I had my bladder removed and my prostate removed. After my surgery, they found cancer cells inside a few lymph nodes but they were just the cells, nothing that metastasized. I'm currently under immunotherapy to battle that situation. However, there was some getting used to being on your ostomy bag and having to live with my life differently. But you know, I'm feeling great, I'm back to work, I got back on the river and fished and rafted and spent times, I got back on the golf course. I think I'm three months post surgery right now and couldn't be feeling better. I'm just, I'm scared and you always think, “Oh, it's too good to be true that where I'm at right now.” I'm really concerned about the cancer cells that are inside of me but feel that my team, my surgeon, the people involved at Huntsman and my support staff back here in Bozeman at the cancer center, we've got a good plan of attack to make sure that I'm staying as healthy as it can be here as long as possible.
Heather Simonsen: It's so good to hear.
Lexi DiPentino: You know, he has his surgeon, Dr. Schmidt, from the Huntsman Center and then his oncologist here in Bozeman, Dr. Hancock. Dr. Schmidt, I could reach out to her anytime if I have any questions and I've had some specific questions. She gave me her email address and it was just so like, she gets back to me right away because, you know, she never sleeps. I'm pretty sure she never sleeps. She's just so caring and the fact that she's helping beyond when we still have our oncologist here and I can just bounce questions off of her and get an answer, it's just that extra is very special.
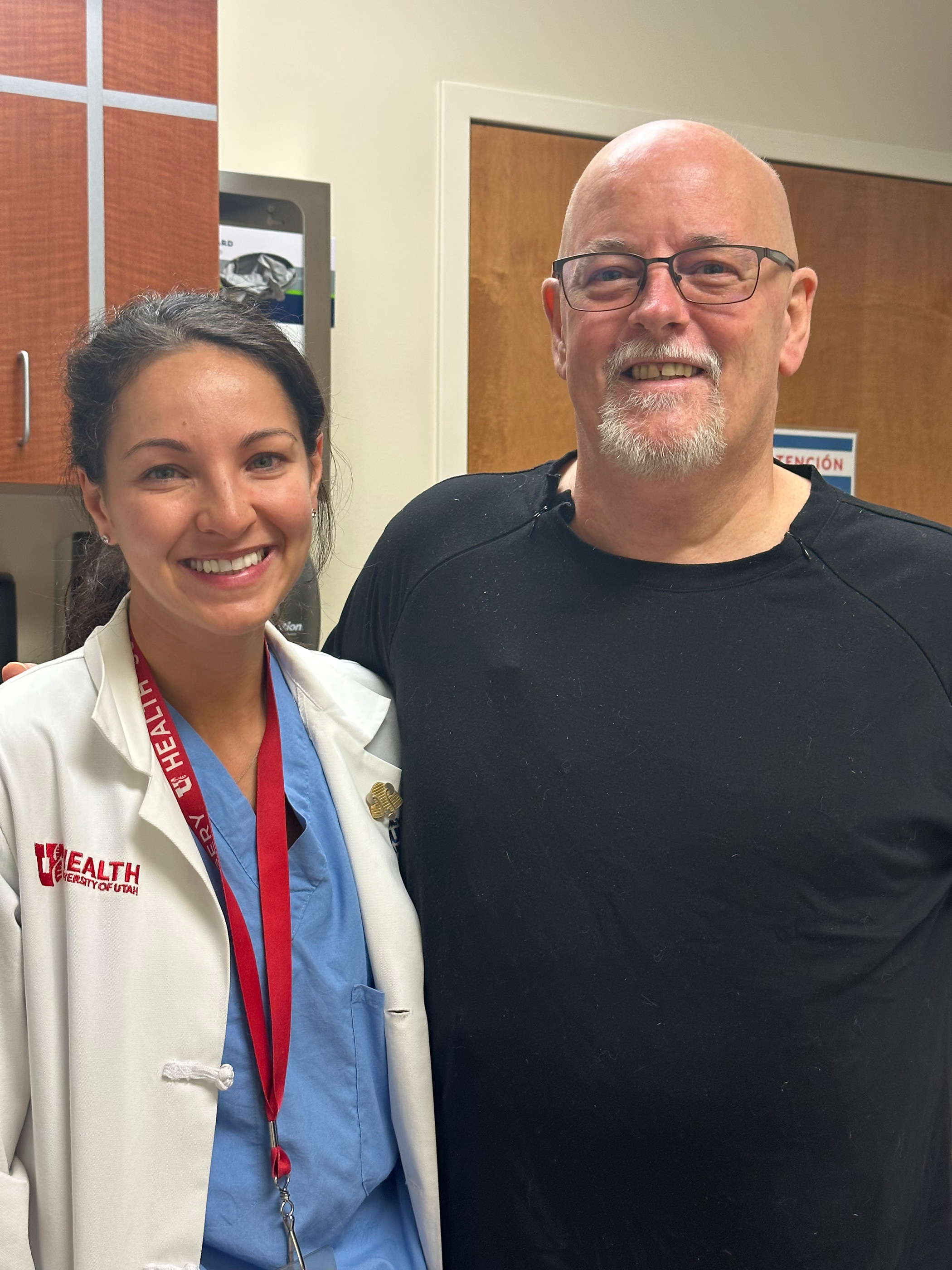
Bogdana Schmidt, MD, MPH, and PJ DiPentino
PJ DiPentino: If I could add to Dr. Schmidt, you know, it's a story in itself is that we live in Montana, where we have our flights scheduled for Friday, we got a hotel set up, we're all set up to get there for my surgery on Monday, and on Thursday, I get a call from Huntsman, “PJ, we're going to have to reschedule.” I went silent and I was “What do you mean?” “Well, your surgeon has been in a bicycle accident and broke his collarbone, and he won't be able to perform the surgery.” I explained to the person on the phone, “Listen, we're flying there, we have we have hotel accommodations, we have rented cars, we can't just change it,” and she was so calm. She said, “Hold on, I'm going to call you back.” She called me back about 30 minutes later and she says, “We have another surgeon Dr. Schmidt. She's doing a surgery in the morning but has agreed to do you and keep everything to the schedule. Everything is on PJ, just get here and we're going to take care of you.” Now, I had never even met my surgeon until an hour before my surgery when Dr. Schmidt came in and introduced herself. I'd be lying if I didn't tell you I Googled her and I checked up on her and found out she was an amazing woman, who had a great reputation at Huntsman and I do believe I lucked out with getting them, no offense to the other doctor. She was wonderful in the way she prepped us for the surgery, showed up with her team, checked on me, took care of me. I truly believe I was blessed. You know, my medical staff, everybody that took care of me from the very beginning to the end, was a woman. I had a woman, the only doctor male I did was Dr. Hancock, who was my urologist, but every single person that I went through my nurses, to staff, Carley, anybody that we interacted with, right down to my surgeon, were females. That couldn't have been any better for me to be blessed with so many caring ladies that took care of me. At one point, I even realized that I told my wife, everyone who's taking care of me has been female! Everyone, every single person. What attests to that as well is that, you know, the medical industry isn't male driven. It's driven by women who care and take care of people.
What does a cancer-free frontier look like to you? (21:13)
Heather Simonsen: PJ, Lexi, before we let you go, I'd like to just ask you a question. We ask all our guests. When you envision a cancer-free frontier, which is the vision of Huntsman Cancer Institute, what does that look like to you? What does it mean to you, when I say we deliver a cancer-free frontier?
PJ DiPentino: It's a second chance. It's a second chance at life. I thank the Lord every day that I wake up and see my children and my wife and my grandson. I worry that I won't be here for long so I'm not going to take advantage of the time that I am here. Huntsman gave me that second chance. There was times I thought, “I'm not going to get through this. I'm not going to make it.” It's just every single thing that we got for news was bad. It never was good. I was like, “Man, I can't believe I can't catch a break.” Well, all that time I didn't know I'd already caught that break and that was going to Huntsman to get my work. And that's for me, that's what it was. It gives me a second chance and the ability to change the way I live. That impact will go on, you know, for the rest of my life as long as they let me hang out.
Heather Simonsen: PJ, Lexi, thank you both so much for joining us. It's been an absolute delight.
Lexi DiPentino: Thank you for having us. We're so blessed and so grateful for being introduced to Amelia. I just cannot all explain to you how she changed our life.
PJ DiPentino: Thank you.
Lexi DiPentino: Yeah, thank you very much.
Welcome, Amelia Thelin, Patient Navigator (22:49)
Heather Simonsen: Thank you both. Well, now we will welcome you properly Amelia Thelin, our rural patient navigator who helped PJ through his cancer. Amelia is part of the frontier and rural navigation program at Huntsman Cancer Institute, which serves people in Montana, Wyoming, and rural Utah, helping them navigate the healthcare system from diagnosis to survivorship. Amelia, we're so glad you're here.
Amelia Thelin: Oh, thank you so much. I'm so excited to be here.
Heather Simonsen: So, what does a patient navigator do?
Amelia Thelin: I mean, you kind of nailed it right off the bat when you said that we help navigate the healthcare system. It can be really complicated, as we talked to PJ and Lexi and heard, especially for those who are having to travel for that care to be far away from family, friends, and support, and all the things that are familiar to them. Just being able to have somebody to kind of connect them with whatever resources they need to be able to get that care. So, navigating the healthcare system, navigating even just the hospital, you know, and on all of the things that come with that.
Heather Simonsen: And how did you become interested in this work?
Amelia Thelin: That's a really good question. My background is, I'm not a health care professional, my background is actually in public education. When I went back to school and got a degree in health education and public health, I wanted to work in a field that would bring meaning to my life. When I left education, I felt like the only way that I could leave the education system, which meant so much to me, is to work in a place and do a job that would have as great an impact on the people that I serve, that I work with, and personal gratification, you know, having that feeling of meaning in the job that I do.
Heather Simonsen: Well it sounds like you achieved that. I saw you tearing up as PJ was describing the way that you helped him. That had to be emotional.
Amelia Thelin: Yeah, that was so touching. They are just the most delightful couple and I was so pleased to be able to work with them. They were referred to me by their social worker in Bozeman. But when I connected with Lexi, first was who I spoke to, there was just a really strong connection there, she was so grateful to have somebody local that she could reach out to and it felt really good to be that person and to be there for them.
Challenges of patients who live far from NCI-designated Comprehensive Cancer Center (25:35)
Heather Simonsen: And let's talk about some of those challenges. Patients who live far away from a National Cancer Institute-designated Comprehensive Cancer Center, like Huntsman Cancer Institute, what are some of those common challenges you see?
Amelia Thelin: Right off the bat, the first thing is just the distance. When people are traveling, there's the transportation to get here, there's the finding the lodging, and things like that the DiPentino’s mentioned. With that travel and that leaving home, there's extra expense with the cost of being able to travel and stay, and even the cost to sometimes their livelihood. When you're local and you have to go to the hospital or to the doctor's office, you're there for a couple of hours and then you go home but these patients that have to travel from Wyoming and Montana, Southern Utah, and other places, they have to take sometimes an entire day to get here and then an entire day to get back. Not to mention, the time that they stay here for their care. That's a lot of time off work, if they're working. It's a lot of time away from their support network, their support system. Then with having rural patients, we're looking at issues with technology, and connectivity, and the digital connection.
Heather Simonsen: There’s so many hurdles and extra challenges that they face. Another one I would imagine to going from small town life to a big metropolitan area, a large cancer center, I would imagine that could cause some anxiety.
Amelia Thelin: Yeah, absolutely. That's something that is really common in the patients that I speak to. That travel between, you know, if you live on a dirt road and you're driving down the road and you see one truck go by it’s a big difference from coming to Salt Lake where as one patient put it, “It's rush hour all the time.” In comparison, so just the driving down here and stuff, that is really anxiety inducing.
Coming from a small rural hospital or clinic where they know every single person that works there, they know their way around, sometimes their entire cancer center is a few rooms in the hospital. To come to the University of Utah and the Huntsman Cancer Institute and have this enormous campus, multiple floors, so many different providers and different people to talk to and to remember and to have phone numbers for and all of that is a lot. It's a lot for our patients.
Heather Simonsen: Well, and PJ and Lexi said you felt like family to them, which I think is such a high compliment to you.
Amelia Thelin: Absolutely.
Relationships with patients (28:20)
Heather Simonsen: How important is that trust that you build with your patients?
Amelia Thelin: Yeah, it is really important. One thing that's a little bit tricky, as Lexi mentioned, the first contact we made was on the phone. It's a little bit tough sometimes to build that rapport over the phone, more so than, you know, a patient that is here in the hospital every day or frequently. Having that connection and having somebody who is there with the boots on the ground, who you can connect with, who when you get there is a familiar voice or a familiar name, you've had a conversation, if not a familiar face yet, just somebody that you feel comfortable with, seems to make a world of difference.
Heather Simonsen: Yeah, I'm not even sure if it can be measured, but feeling that peace, and that calm, and that connection has to make such a difference.
Amelia Thelin: Yeah, I had one patient the other day who was, well it was the caregiver, the wife of a patient, when I was speaking to her over the phone, the first phone call that we had, she was feeling very, very anxious about the treatment and coming to the hospital and all the things that we've talked about. I reassured her like, “When you get here I'll watch for you to check in, and I'll come down and say hello and see if there's anything that I can do to help you.” I came down and met them, she said to me, like mid-sentence, she stopped and she said, “Do you know what you did?” I was kind of taken aback, and she said, “You have taken all of my anxiety away.” She felt so anxious, and just having a person to connect with made a huge difference. I think that one of the key differences with a navigator that is different from speaking to a provider is, as I mentioned, I don't come from a medical background, a healthcare background. As a lay navigator, is what we're considered, patients sometimes feel a little bit more comfortable asking their questions that they wouldn't necessarily ask their provider that they don't feel comfortable, or they don't want to take too much of their time, because they know that they're very busy, and things like that. They know that they can sit and have a conversation with me and if I don't know the answer to the question that they have, they know that I can find it, and we'll get it for them.
What needs to be done to treat patients in their own home towns? (31:14)
Heather Simonsen: Well I think you bring up such an important point, I mean, that it's those little things that make a big difference. I'm so grateful that you shared that. Ideally, you know, as a part of our mission and at Huntsman Cancer Institute, we'd really like to be able to treat these patients where they live and make it possible. That's the goal for them to stay in their homes, in their communities with their families. What do you think still needs to happen in order to do that?
Amelia Thelin: Well, that's a really good question. I know that we've, you know, thankfully, through the pandemic, we've increased the ability to do telehealth and taken away some of the barriers there, but there is often still that barrier of just the technology. A lot of our patients that are coming from rural areas, they don't have high speed internet, or the bandwidth even to have that connection. I don't know if it's a Huntsman thing necessarily, but just building up that infrastructure so that patients can do that remotely and digitally. Then, removing some of the blockades with insurance issues and Medicaid issues and things like that going across state lines.
Heather Simonsen: Well, exactly, because if you go across state lines for treatment, it can be a lot more expensive.
Amelia Thelin: Right, and sometimes insurance doesn't cover it or doesn't cover very much when you're going to another facility, so yeah, that's really crucial.
Heather Simonsen: There are still a lot of hurdles and work that needs to be done, that infrastructure, as you mentioned, that the bandwidth and truly this is lifesaving work, this needs to happen. Wouldn’t you agree?
Amelia Thelin: Yeah.
Most rewarding about being a patient navigator (33:11)
Heather Simonsen: What is the most rewarding part of your job?
Amelia Thelin: Well, hearing from people like the DiPentino’s certainly, and they're not the only patients that I've had that connection with. Each patient is unique and they're all in a place where they really need that gentle guidance, that hand to hold, and a friendly voice, and a friendly face. You know, one of the things that's really rewarding is when I speak to a patient and I'm able to connect them with resources that they didn't even know existed. PJ and Lexi mentioned that they weren't even aware of the Hope Lodge from the American Cancer Society. Having a resource like that at our disposal to be able to say, “Hey, there's this lodging that you can, that you can reserve that is not going to cost you anything.” There are other organizations that provide free air transit, for patients and their caregivers. And being able to connect patients with things like that really have an impact on their lives and on their care is really rewarding.
What does a cancer-free frontier mean to you? (34:20)
Heather Simonsen: Finally, Amelia, I'd like to ask you the question, we ask everyone on our podcast. What does it mean to you to deliver a cancer-free frontier?
Amelia Thelin: You know, personally, I have family members who have battled cancer, and to be able to eliminate that from other loved one’s lives is just an incredible idea and concept. Additionally, there's so many other concerns and things to worry about in the world. If we could eliminate cancer and have those resources to focus on, there's so many other worthwhile and worthy needs out there. Think of all the good that we could do.
Heather Simonsen: That’s beautiful. Thank you for sharing that. Amelia Thelin, it's been such a joy having you on the podcast and thank you for your incredible work. You're the boots on the ground that make it all possible, so thank you.
Amelia Thelin: Yeah, thank you very much.
End Credits (35:29)
Heather Simonsen: We extend our sincere gratitude to PJ and his wife, Lexi, and Amelia Thelin, for sharing their expertise and experiences with us today. Traveling far distances for care can make a cancer diagnosis even harder. Huntsman Cancer Institute is working to bridge the gap for patients who live in the countryside through rural patient navigators. But there's so much that still needs to be done. Coming up in part two of this episode, we'll talk about the solutions. Our guest will be one of our investigators, and he's got an amazing story to tell. An outing at a public pool and a chance meeting saved his life and shaped his career. That's next time.
To our dedicated listeners, we appreciate your support. For additional resources, be sure to check out the show notes, and if you want to stay connected with us and be the first to know about upcoming episodes, don't forget to hit that subscribe button on your favorite podcast platform. We truly appreciate it if you could take a moment to leave us a rating or review. Your feedback is incredibly meaningful. And please tell your friends and family about our podcast and share episodes on social media. We're always eager to hear from you whether you have questions, comments, suggestions for future topics, or a personal story you'd like to share, please visit our website huntsmancancer.org. I'm your host and executive producer of the cancer free frontier, Heather Simonson, Avery Shrader is our producer, with help from Carley Lehauli and Jill woods. A special thanks to the pod mill and Mix at Six Studios for their help with this episode.
