Call 911 Immediately If You Experience Stroke Symptoms
Why Choose University of Utah Health for Exceptional Stroke Care?
Our Stroke Center is a national, DNV GL-accredited leader in comprehensive stroke care. We are a dedicated team specializing in stroke treatment and available 24/7 for our patients. Our center offers an accredited specialty stroke rehabilitation program as well as providing care to rural and underserved areas via Telestroke (telemedicine).
At University of Utah Health, the Division of Vascular Neurology specializes in stroke care with our faculty and fellows conducting research that makes our success possible.
1,600+
urgent stroke consultations per year
REGION'S FIRST
Comprehensive Stroke Center
ONE OF THE NATION'S LARGEST
telestroke network
Find a Stroke Specialist Near Me

"I started talking right when they pulled the clot out. It was just crazy. It was a very special moment for a lot of people because we got to see the miracle of medicine, how [doctors] can just make one right treatment decision and totally change somebody's life."
Stroke Programs
Stroke Rehabilitation
Our highly trained stroke experts at Craig H. Neilsen Rehabilitation Hospital use state-of-the-art technology to help restore order in your life after a stroke. The Stroke Rehabilitation program ensures that the care you receive at U of U Health is among the best in the nation.
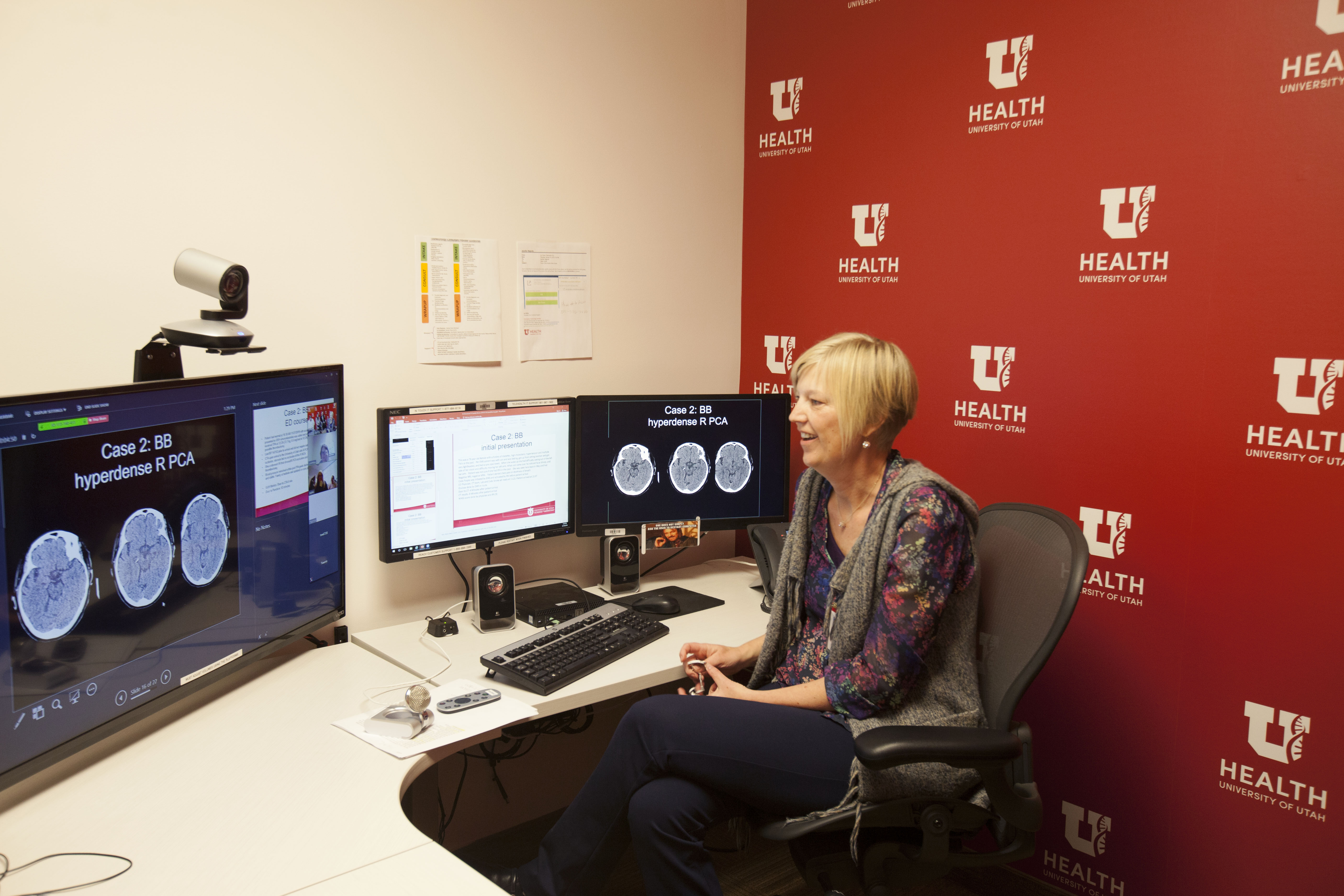
Telestroke Program
Using real-time videoconferencing and teleradiology, U of U Health's TeleStroke Program provides 24-hour on-call neurologists to community hospitals to help with diagnosis and treatment of stroke patients.
Stroke Treatment We Provide
Our comprehensive Stroke Center offers stroke treatments, such as medications and/or life support treatments administered by emergency-trained personnel:
- Machines to assist breathing
- IV fluids
- Blood pressure control
Our providers also perform surgery after a stroke has occurred or to prevent a future stroke. The best treatment that we can apply ourselves is preventive treatment. Consult your provider and study the signs of stroke to be prepared.
Meet Our Patients
WATCH WHITNEY'S STORY
When Whitney Meyers got to the top of her stairs, she felt dizzy and needed to lay down. She couldn't get off the floor and asked her children to get her sister for help. When her sister arrived, Whitney's face had drooped to one side—a telltale sign of a stroke.
Want to Participate In a Clinical Study?
Clinical trials and research studies help our physicians and researchers prevent, diagnose, and treat diseases.
Find a Stroke Clinical TrialRFVIIA for Acute Hemorrhagic Stroke Administered at Earliest Time (FASTEST) Trial
U of U Health is conducting a research study of the emergency treatment of patients with bleeding in the brain also called intracerebral hemorrhage. We are asking community members to think about this research and let us know what you think about the FASTEST study.