From Volume to Value in Health Care - JAMA editorial
Listen to the podcast with University of Utah CEO Vivian Lee and health care strategeist Michael E. Porter
(SALT LAKE CITY) - Bucking national trends, a new study suggests that a program could be making a difference in healthcare quality and cost. Developed by University of Utah Health Care (UUHC), the value driven outcomes (VDO) program breaks down health procedure costs to the level of each bandage and minutes of nursing time, revealing variabilities that are otherwise hidden from view. After a multidisciplinary care team addressed inefficiencies in three common procedures - joint replacement, in-hospital laboratory testing, and sepsis management – VDO showed that patients fared better and costs in some areas fell by about 10 percent. The results were published online in the Journal of the American Medical Association (JAMA) on Sept. 13.
"The transition of health care from volume to value is no longer theoretical, or wishful thinking," states an accompanying editorial written by health care transformation leaders, Michael E. Porter, Ph.D., a Harvard Business School strategist, and Thomas Lee, M.D., M.Sc., chief medical officer for Press Ganey Associates. "This article shows that achieving better quality and lower costs is possible, and everyone can benefit: patients, hospitals and physicians, and society."
"In order to provide higher value care, we need to better understand our costs," explains lead author Vivian S. Lee, M.D., Ph.D., M.B.A., senior vice president at University of Utah Health Sciences and CEO of UUHC, which has 1.7 million patient visits each year. "We're making the case that an organization can quantify and manage value, and that's going to be a huge part in improving the health care system."
A case in point: knee and hip replacements, which - along with the likes extensive burns, Cesarean deliveries, and drug and alcohol abuse - was placed on a list of 19 procedures with the highest total direct costs. Given this, along with the relative standardized nature of joint replacement surgery and quality efforts already underway with joint replacement providers, the VDO tool offered an ideal opportunity to assist the team in further care process improvements.
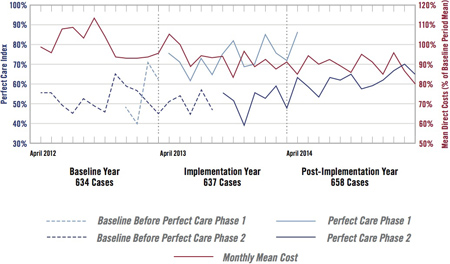
The team of multidisciplinary Joint Replacement clinicians met and identified key care pathway improvements that would likely have an impact on the time a patient spends in the hospital (length of stay), the quality of care the patient received, the cost of care and even the cost of implants. Using the VDO tool, they identified cost and locally and nationally defined quality metrics, termed the "Perfect Care Index", and followed the index to determine if the clinical pathway improvements were making a difference.
For example, the team found that a certain percentage of patients were not meeting Perfect Care because they were not up and out of bed on the day of surgery, a locally defined quality metric. One commonality was that these cases occurred late in the day, after physical therapists shifts ended. After adjusting the therapists' shifts they achieved 100% compliance with Perfect Care for that measure, and saw that it was a significant predictor of length of stay and reduced cost. Simple changes like this one, and negotiating improved pricing for implants, showed improvements. Length of stay decreased from 3.5 to 2.9, and costs decreased by approximately 10 percent.
"We were able to get a macro-level view of where the opportunities for improvement were," says senior author Robert Pendleton, M.D., chief medical quality officer at UUHC. "The case studies were driven by doctors having insights and having data available."
Two additional, common procedures saw similar changes. In the case of in-hospital lab testing for acutely ill patients, it was found that some health care providers were ordering unnecessary tests. An education campaign and other measures drove down superfluous testing, decreasing mean costs from $138 to $123, or 10 percent, per day. In a pilot project for management of sepsis, one of the top three killers in hospitals, raising awareness of warning signs contributed to a shortened mean time to administering potentially life-saving antibiotics, from 7.8 to 3.6 hours.
"We have great data, but this is just the beginning," says Pendleton. The program is expanding to optimize other procedures, and new versions of VDO are factoring in additional measurements such as patient reported outcomes that take into account the patient's own point of view of how well they are doing.
"I feel like by the time I retire I'm going to think, ‘Oh my gosh, how could we have not even been thinking about value and quality back then? It's hard to imagine,'" says Lee.
###
"Implementation of a Value-Driven Outcomes Program to Identify High Variability in Clinical Costs and Outcomes: Association With Reduced Cost and Improved Quality" was published in the JAMA online on Sept. 13, 2016
Study authors are Vivian S. Lee, Kensaku Kawamoto, Rachel Hess, Charlton Park, Jeffrey Young, Cheri Hunter, Steven Johnson, Sandi Gulbransen, Christopher E. Pelt, Devin J. Horton, Kencee K. Graves, Tom H. Greene, Yoshimi Anzai, and Robert C. Pendleton all from University of Utah Health Care.