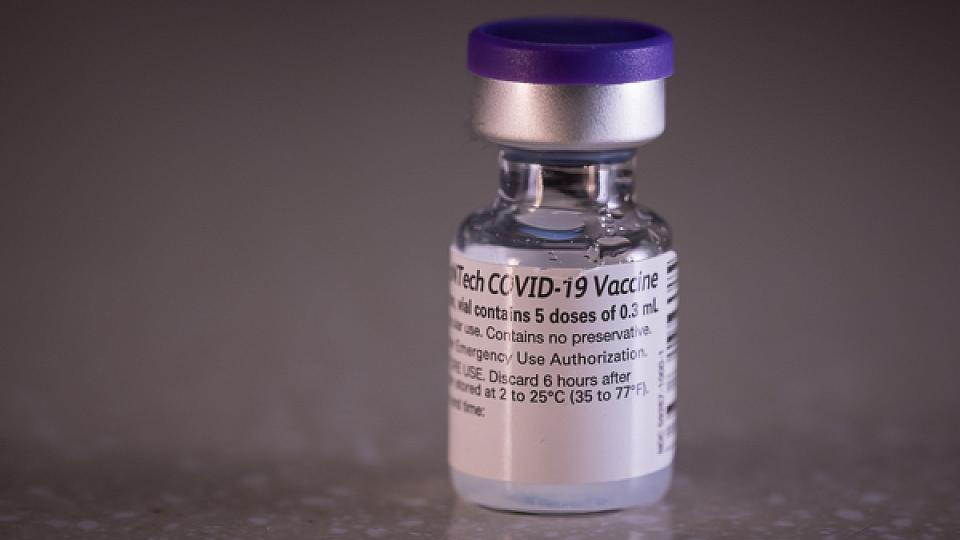
Coronavirus Vaccine
Safe & Effective Vaccines for COVID-19
Vaccines for COVID-19 help reduce damages from the coronavirus pandemic. The vaccines:
- help fewer people be infected.
- lower the number of people who have to be cared for in the hospital.
- reduce the long-term effects of COVID-19.
- lower the number of deaths from COVID-19.
The Pfizer/BioNTech and Moderna mRNA vaccines are authorized for use for people ages 6 months and older.
COVID-19 Vaccines & Booster Shots Available
Stay up to date on your COVID-19 vaccinations and booster shots. Visit vaccines.gov to find your nearest vaccine provider or call 1-800-232-0233. U of U Health patients can ask for the COVID-19 vaccine or booster shot at their next appointment.
Vaccine Side Effects
Side effects are a sign that your immune system is building up protection against disease. Side effects for the COVID-19 vaccines include:
- Mild pain, swelling, or redness at the injection site where you get the vaccine
- Fever, usually mild and short-lived
- Chills
- Feeling tired
- Headache
- Muscle and joint aches
- Diarrhea (seen in Pfizer/BioNTech clinical trials)
- Nausea (seen in Moderna clinical trials)
- Swollen lymph nodes in the same arm as the injection site (seen in Moderna clinical trials)
Some people who received the vaccine reported worse fevers and aches than others. Side effects were usually short-lived and able to be managed with fever-reducing medications, such as Tylenol. For people who received the Pfizer/BioNTech or Moderna vaccine, side effects were more common after the second dose than the first dose.
Heart Inflammation Symptoms
There have been rare reports of people—particularly male adolescents and young adults—who received the mRNA vaccines (Pfizer/BioNTech & Moderna) and experienced symptoms of myocarditis or pericarditis (heart inflammation conditions) within several days of getting their shot. This rare adverse reaction occurred more often after the second dose of vaccination. With proper treatment and care, most patients saw their symptoms improve quickly. However, it's important to keep in mind that the known risks of COVID-19 illness, such as long-term health problems, hospitalization, and even death, far outweigh the risks of having a rare adverse reaction to the vaccines.
Allergic Reactions to Vaccines
Severe allergic reactions or anaphylaxis to vaccines are extremely uncommon. If a severe allergic reaction does occur, it typically happens within a few minutes to one hour after receiving the vaccine. However, some people have experienced non-severe allergic reactions (i.e., hives, swelling, and wheezing) within four hours after getting vaccinated.
You should not get the COVID-19 vaccine if:
- You have had a severe allergic reaction after the first dose of the Pfizer/BioNTech or Moderna vaccine.
- You have had a severe allergic reaction to any ingredient in the vaccine.
- You are allergic to polyethylene-glycol (ingredient in Pfizer/BioNTech and Moderna vaccines).
For a list of vaccine ingredients, see the Moderna or Pfizer-BioNTech fact sheets.
People with a history of immediate allergic reactions — even if it was not severe — to other vaccines or injectable therapies should consult with their doctor before getting the COVID-19 vaccine, according to CDC recommendations.
I Had COVID-19. Should I Get the Vaccine?
The length of time that you are protected from getting COVID-19 again after infection varies from person-to-person. Health experts recommend you get the vaccine even if you have been infected by COVID-19. CDC guidelines say you may delay your vaccine for three months after having COVID-19.