What Is Lymphedema?
The human body has three types of vessels, or tubes, that blood flows through: arteries, veins and lymphatics. Lymph is the clear fluid part of blood and contains water, proteins, and immune cells. Lymph flows from the spaces in-between your cells, into lymphatic vessels, and back to veins that return to your heart.
If arteries and veins are the superhighways for blood flow in the body, lymphatic are the small side roads.
Lymphedema is swelling in a part of your body where lymphatic fluid builds up more than normal. It can develop when lymph nodes are removed or when lymph vessels that carry lymphatic fluid are missing, damaged, or not developed.
When lymph fluid does not drain properly, it causes swelling in any part of the body, most commonly in arms and legs. Other common sites for lymphedema are the genital areas, head, neck, and abdomen.
Eligible Patients for Treatment and Referrals
You must meet the following requirements if you have a previous cancer diagnosis:
- Complete therapies (such as physical therapy, occupational therapy, or compression) for six months before seeing a lymphedema surgeon
- Have a current BMI of less than 40
- We will consider exceptions for this if your referring provider writes us a letter addressing BMI.
You must include the following items in your referral if you have not had a previous cancer diagnosis:
- A report and/or images confirming your lymphedema diagnosis
- Nuclear medicine lymphoscintigraphy testing
- Records showing you've completed six months of therapy (such as physical therapy, occupational therapy, or compression)
- A current BMI of less than 40
You must send your referral to a lymphedema specialist before making an appointment.
Fax: 801-581-5794
What Causes Lymphedema?
- Having lymph nodes removed or radiation due to cancer: This is the most common cause of lymphedema in the United Stated and other developed countries. The most common types of cancer associated with lymphedema are breast (arm lymphedema), gynecological cancers including cervical, uterine, ovarian, vulvar (leg lymphedema), prostate and other urological cancers (leg lymphedema), melanoma (arm or leg lymphedema) and other skin cancers. Radiation damages the small lymphatic vessels and can lead to lymphedema where the lymph nodes have been removed.
- Trauma or surgery: Both trauma and surgery can injure lymph vessels and lead to lymphedema.
- Present at birth (congenital)/inherited: Lymphedema that is present at birth is also called primary lymphedema. It is estimated that one in 6000 people is born with insufficiency of the lymphatic system. You may develop lymphedema at any point during your lifetime from infancy to late adulthood, without any apparent cause. This type of lymphedema can be inherited.
- Obesity: Extreme obesity can cause lymphedema. However, several studies have shown that any degree of obesity increases the risk of lymphedema in cancer survivors.
- Parasites in underdeveloped countries: A parasitic worm called, filaria, can cause lymphedema in infected patients. This is the most common cause of lymphedema in the world.
What Are the Symptoms of Lymphedema?
Symptoms of lymphedema include the following:
- Swelling or puffiness, usually in the legs or arms, but can be seen in genitalia, trunk and face
- Indentation or pitting of skin that stays longer than normal; for example, after removing socks or rings
- Feeling of fullness, heaviness, tightness, or pressure
- Tingling sensation or numbness
- Pain or discomfort
- Difficulty moving your joints due to swelling
- Feeling warmer
- Hard, abnormally dry, textured, or scaly skin
- Recurrent infections or skin rashes
How Is Lymphedema Diagnosed?
A medical professional, such as a doctor, certified lymphedema therapist, or physical therapist, diagnoses lymphedema. Unfortunately, doctors often overlook lymphedema and the patient receives treatment at very late stages.
It is important to talk to your doctor when you have any symptoms, especially if you have recently had cancer surgery, radiation, traveled to an area where filariasis parasites are common, or have a family history of lymphedema.
To diagnose lymphedema you will have a clinical exam and imaging. The imaging uses indocyanine green (IcG) dye to show the structure and functioning of the lymphatic system.
This imaging can be done in the clinic by injecting IcG dye into the webbed spaces of your fingers and toes. Then we take images of the affected area with a special camera. Other useful imaging tests include lymphoscintigraphy, MRI, MR lymphography, and bioimpedance spectroscopy.
Early Stage Lymphedema
Early stage lymphedema can be difficult to diagnose. Patients usually complain of a feeling of heaviness, tingling, and swelling. If you can catch lymphedema early, you can prevent it from being a chronic and debilitating condition.
It is very important to adequately diagnose this condition and start treatment early.
What Are The Available Treatment Options?
Common treatment options include exercise, compression garments, and physical therapy. Advances in microsurgery over the past 20 years have greatly increased the available treatment options.
Patients at different stages may require different types of treatment or a combination of procedures. The available surgical treatment options include the following:
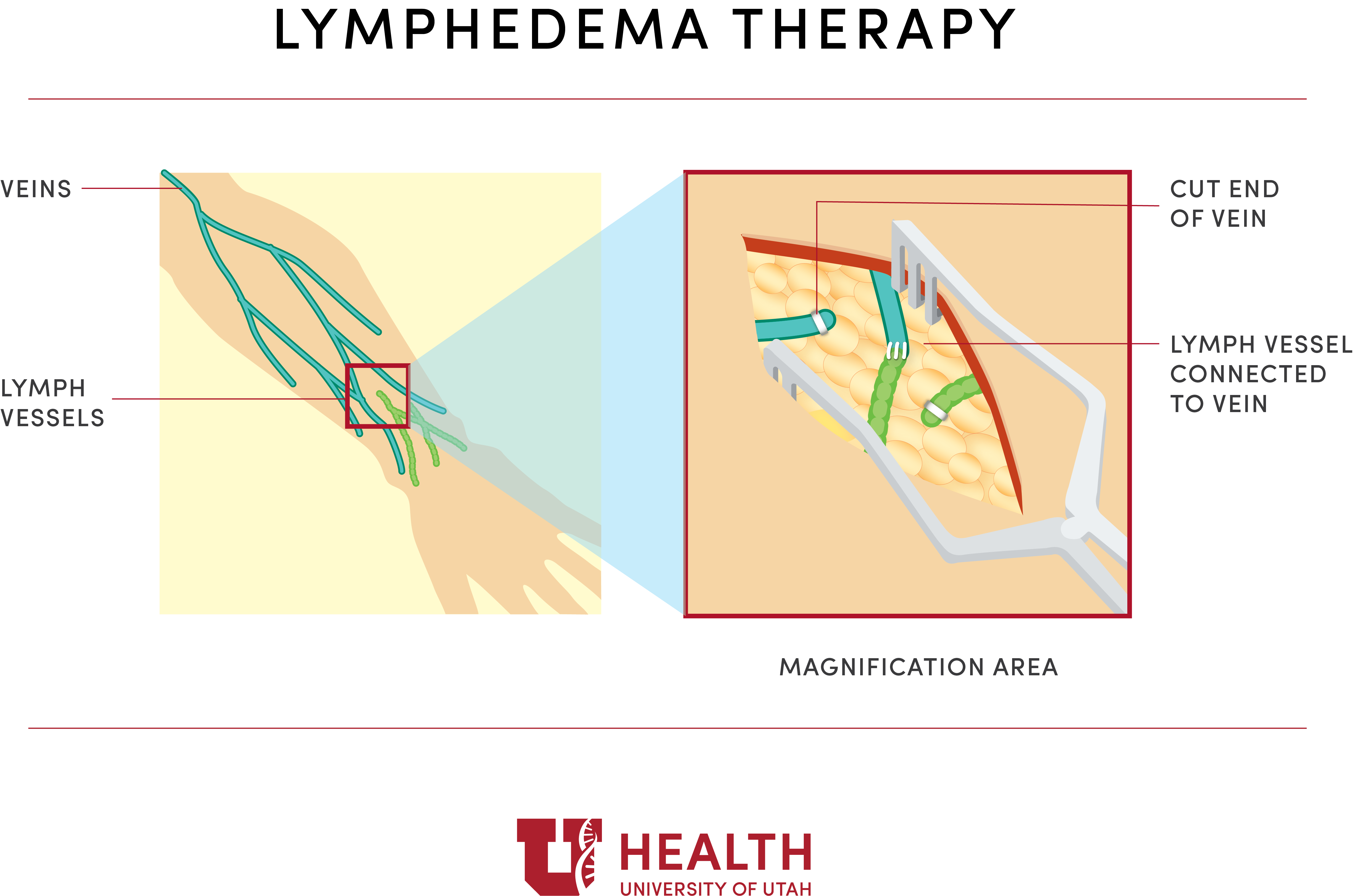
Lymphovenous Anastomosis (LVA) or Lymphovenous Bypass (LVB)
This procedure uses super microsurgery to connect lymph vessels to veins. We re-route excess lymphatic fluid to the venous circulation. This way we can bypass damaged or removed lymph nodes.
During this surgery, your surgeon makes a few small cuts on the skin, and then connects the tiny lymphatic vessels to nearby veins. This can be done with minimal damage to the tissues around the lymphatic vessels.
We usually perform LVA surgery as an outpatient surgery with short recovery time.
Vascularized Lymph Node Transplantation (VLNT)
In this procedure, your surgeon takes lymph nodes from another part of your body, such as the abdomen or neck, and transfers them to the affected area to reconstruct the lymphatic system.
Specialists use microsurgery to connect the blood vessels that suppy the transferred lymph nodes to blood vessels in the area of lymphedema. These transplanted lymph nodes develop new lymphatic vessels that absorb excess fluid and decrease lymphedema in the surrounding tissue.
This is an inpatient surgery with a hospital stay of two to four days.
Liposuction
Lymphatic fluid stimulates fat formation and inflammation in the surrounding tissues. In advanced lymphedema, the affected arm or leg becomes swollen and hard due to fat deposits. Liposuction removes fat tissue and reduces the size of the arm or leg.
Liposuction for cosmetic reasons is different than liposuction for lymphedema. Not every plastic surgeon who performs liposuction is qualified to perform liposuction for lymphedema.
This surgery is typically done as an outpatient (you can leave the same day). We do require patients to wear compression garments after surgery.
Debulking Procedures
In very advanced stages of lymphedema, an entire arm or leg may swell to several times its normal size. Your skin can also develop a dry, thickened, pebbly appearance.
A debulking procedure removes all swollen tissue through surgery. We then place skin grafts to close the wound. This is also called the Charles Procedure.
Lymphedema Therapy
Your physician may suggest lymphedema therapy as initial treatment or in combination with surgery. A certified lymphedema therapist is either a physical therapist or an occupational therapist with additional lymphedema training. Lymphedema therapy helps reduce swelling and keeps it at a manageable level so you can carry out your daily activities.
Lymphedema therapy involves the following:
- wearing compression bandages,
- manual lymphatic drainage (a type of light pressure massage), and
- physical exercises depending on the location of the swelling.
Therapy sessions occur at least once a week for about four to eight weeks. You will be asked to complete the exercises you learn in session at home. You may also receive a compression garment or a pneumatic compression device (pump) to help keep the swelling down in between therapy sessions and to continue long-term after you complete lymphedema therapy.
Is There a Cure For Lymphedema?
Exercise, compression garments, and physical therapy can help control the symptoms and prevent lymphedema from getting worse. Although they do not cure the disease, they are often helpful with or without surgery.
Most surgical procedures like LVA and VLNT will help to remove symptoms, reduce the size of the affected area, and increase quality of life. These procedures typically do not cure lymphedema. However, LVA has been shown to cure lymphedema in a small percentage of patients who were in the early stages.
Can You Perform Surgery to Prevent Lymphedema Before It Develops?
We can perform surgery to prevent lymphedema. In collaboration with oncology surgeons at the University of Utah, we are offering LVA at the time of lymph node removal surgery.
This technique is referred to as LYMPHA (Lymphatic Microsurgical Preventative Healing Approach). During cancer surgery where specialists remove the lymph nodes, we find lymph vessels and immediately re-route them to a nearby vein. This can prevent lymphedema in many patients.
However, a small percentage of patients still develop lymphedema. We will closely monitor you after surgery for the development of lymphedema. We will intervene as early as possible if lymphedema develops.
The University of Utah is one of the few centers in the country that provides multidisciplinary lymphedema care—meaning we work with other specialists to give you the best care possible.
Find a Specialist
What Is the Consultation Process Like?
You may self-refer or be referred by your doctor.
At your appointment, your surgeon will discuss your history and perform a physical exam. We will take limb measurements in areas with and without lymphedema. We may also take clinical photos—with your consent.
Your specialist may order specialty imaging as well. You will have a detailed discussion with your surgeon of the options for your lymphedema care, and we will create a plan with your input.
We can also make referrals to physical therapy or oncology if you need them.
Hear From Our Patients
A year after her total knee replacement, Liz’s knee continued to swell when it should have been healing. Despite her worsening symptoms and pain, her doctors weren’t too concerned. One morning, she saw a U of U Health plastic surgeon talking about lymphedema on the television. The symptoms sounded very similar to what Liz had been experiencing so she scheduled an appointment with U of U Health to get some answers. A diagnostic test confirmed she had lymphedema.

Huntsman Caner Institute Awarded LE&RN Center of Excellence Designation
Huntsman Cancer Institute at the University of Utah led by Fatma Tuncer, MD has been awarded the LE&RN (Lymphatic Education and Research Network) Center of Excellence designation.
