
Over the past three decades, Moran Eye Center’s Nick Mamalis, MD, and Liliana Werner, MD, PhD, have vetted some of the most innovative devices in eye care.
Intraocular lenses (IOLs) replace the eye’s own natural lens for more than 6 million people—most of them cataract patients—around the globe each year. There’s hardly one on the market that hasn’t been tested at the duo’s nonprofit Intermountain Ocular Research Center at the John A. Moran Eye Center.
While the invention of the IOL dates back to the 1940s, the device is still going through myriad refinements: companies worldwide send the center a steady stream of prototypes and materials in an industry projected to reach $4.7 billion in the U.S. by 2020. The race to develop the "perfect" IOL has created a complex landscape of choices for both doctors and their patients, but the latest technology to arrive in the Mamalis Werner lab—laser-assisted Refractive Index Shaping (RIS)—could change all that, and more. To grasp the revolutionary nature of RIS, one must understand the challenges of IOLs from a surgeon’s perspective.
‘WE’RE STILL DEALING WITH HUMANS’
In the U.S. alone, cataract surgery accounts for 3.2 million outpatient procedures each year, and it’s one of the safest and most effective surgeries available. Even so, ophthalmologists must help patients choose the IOL that’s right for them.
Surgeons like Mamalis want to give their patients both distance and near vision after surgery. For that, selecting a so-called multifocal or ‘premium’ IOL might be best, although unwanted visual side effects such as glare can occur. Choose a monofocal IOL, and the patient must commit to wearing eyeglasses after surgery.
Beyond selecting IOL type, calculating how powerful its refractive properties should be isn’t an exact science.
"Although techniques for measuring the length and shape of the eye and the formulas for calculating the power of the IOLs themselves are getting better, it’s still not perfect," said Mamalis. "The problem is that even when we use the best measurements, the best formulas, we’re still dealing with humans. That means there are still going to be some people that end up not having the proper result."
In some cases, an IOL can later shift its position inside of the eye. Dislocations might be prompted by eye trauma, eye diseases that weaken the tissues holding the lens in place, or even complications from other eye surgeries. Removing an IOL isn’t optimal: the procedure carries a higher risk for complications.
THE NEXT BIG LEAP
But what if physicians had several opportunities to adjust the IOL power and type weeks and even years after placing it into a patient’s eye—all without making a single incision?
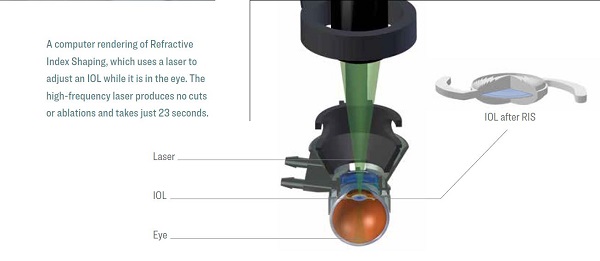
Therein lies the appeal of RIS, laser technology owned by California-based Perfect Lens, LLC. The RIS Perfector laser uses ultra-short pulses to induce a chemical reaction that changes the IOL in just 23 seconds and produces no cuts or ablations on the eye. The result could be incredibly accurate vision. A 2016 study by Mamalis and Werner found RIS to be both biocompatible and extremely accurate, producing IOL power within .01 diopter of its target. That translates into a level of accuracy better than eyeglasses can produce.
The possibilities don’t end there.
"Let’s say a patient already has a multifocal lens, but doesn’t like it," said Werner. "With this technology, you could erase what’s already on the lens and switch to something else."
When might RIS be available for patients? Mamalis and Werner are now conducting a second, six-month biocompatibility study that could lead to FDA approval to take RIS into clinical trials at Moran.
A ‘DISRUPTOR’ FOR INDUSTRY
The driving motivation for ophthalmologists to adopt RIS is improving sight—for patients, it may be their pocketbooks. U.S. health insurers that cover cataract surgery don’t often foot the bill for anything other than a monofocal IOL.Those who can afford it pay thousands out of pocket for premium lenses with additional features, including multifocal IOLs.
Perfect Lens CEO Steven Smathers said RIS could reduce costs, allowing patients to choose a basic, low-cost IOL covered by their insurer. Then, they’d pay a few hundred dollars to have its power and features adjusted through RIS.
"It’s game-changing technology for the industry," said Smathers, "but attractive for patients."

RIS Could be Life Changing for Pediatric Patients
Four months after her premature birth, Isabella Garcia has already undergone cataract surgery in one eye.
Now, Moran pediatric specialist, Leah Owen, MD, PhD, is teaching Isabella’s mother, Klarita Garcia, how to place a tiny contact lens in her baby’s eye.
"Isabella’s eye will grow a lot before she reaches school age, when we can implant an IOL," explained Owen. "But since we can’t change the IOL power once it’s in the eye, we have to ‘over-power’ the IOL so she can grow into it."
That means multiple contact lens changes and strong glasses. "All these moving parts must be constantly assessed because it’s a very important time for the brain to learn vision," said Owen.
RIS would enable Owen to easily adjust the IOL as Isabella grows. The idea that her daughter could grow up with better vision and face fewer eye surgeries as an adult is an amazing prospect for Klarita Garcia.
"I’m so glad technology is advancing and that this could be a possibility," she said. "Getting such good care and medical treatment is why our daughter is here with us today."