
Editor's Note: This article is based on interviews conducted in 2020 and first appeared in Moran's 2020 Focus annual report.
ELCHE, Spain—At the age of 58, Berna Gomez has lived the past 16 years of her life in total blindness.
She was not able to take one last glimpse of the school where she worked as a teacher for more than a decade before her career was cut short. She did not see the faces of her two sons change and mature as they grew into men. She cannot take in views of the orange trees in the foothills of Valencia on her daily walks or look into her husband’s eyes.
But in late 2018, inside a university research laboratory, a single bar—a white line made from white light—appeared on the midnight canvas of her mind. In a quiet, nondescript room filled with scientists who had created the image using a tiny microelectrode array implanted in Gomez’s brain, she exclaimed, "I can see something!"
Underlying her awe was the joy of a shared experience. The scientists could see a line drawn on a poster board in the lab; now, she could see one, too.
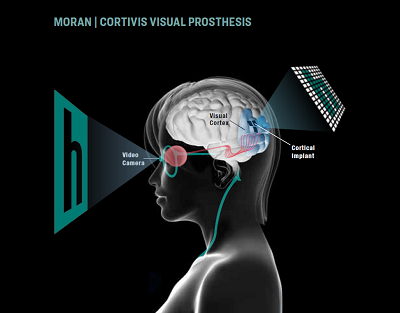
Gomez was successfully testing the Moran|Cortivis Prosthesis, developed by John A. Moran Eye Center and University of Utah biomedical engineering researcher Richard "Dick" Normann, PhD, to create artificial vision, for the first time. Profoundly blind users without any vision wear eyeglasses equipped with a miniature video camera; specialized software encodes the visual data and sends it to the implanted microelectrode array to create images in the visual cortex.
While an international research team collaborates to push the science forward, its progress is dependent on the bravery of people like Gomez.

"This [prosthesis] could give a blind person more mobility. It could allow them to identify a person, doorways, or cars easily. It could increase independence and safety. That’s what we’re working toward."
Richard "Dick" Normann, PhD
The Collaboration to Create Artificial Vision
At the Elche campus of Miguel Hernandez University in Spain, Eduardo Fernandez, MD, PhD, runs a bioengineering lab of 20 scientists working on various projects in close collaboration with Hospital IMED Elche—artificial vision among them.
In his office and on computer screens in the lab are images of his Moran collaborators and mentors, bioengineer Normann and retinal neurocircuitry expert Helga Kolb, PhD. Working with a team of neurologists, psychologists, engineers, physicians, and surgeons, Fernandez and Normann are now putting decades of research needed to create the prosthesis to the test.
For Fernandez, the work is part of his life’s dream to help patients, sparked during his time completing postdoctoral work at Moran in the 1990s.
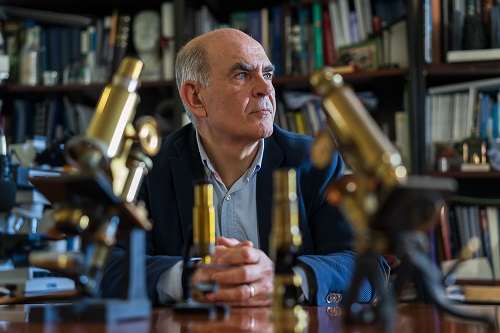
"During that time, I went to a talk on artificial vision given by Dick," said Fernandez, now a Moran adjunct research professor. "For me, it was really amazing. For the first time in my life, I heard people were working on artificial vision. That was 30 years ago, and Dick and I have been collaborating ever since."
Fernandez met Gomez in 2007, during research he was conducting using transcranial magnetic stimulation. In that study, Normann and Fernandez used an electromagnetic coil placed on her scalp to stimulate neurons in the visual cortex to produce phosphenes, or white flashes of light that both sighted and blind people can perceive. Gomez was exceptionally good at describing the phosphenes, even though they appeared for only a split second.
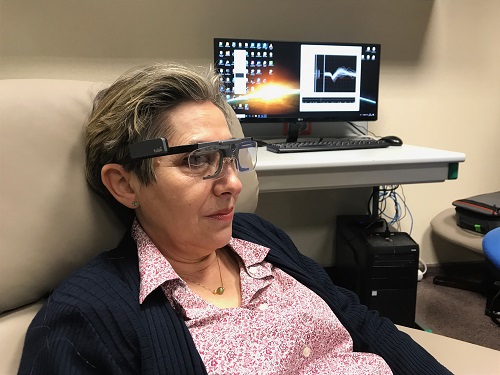
Years later, Fernandez reached out to Gomez to test the visual prosthesis. The effort, he told her, would involve brain surgery and months of intense experiments that would require her to temporarily relocate from Valencia to Elche. The primary goal was to evaluate safety, he said, but the research team hoped the prosthesis would turn video input into images constructed of phosphene patterns that Gomez could perceive.
Gomez would be the first person in the world to have a key part of the prosthesis—Normann’s famous Utah Electrode Array (UEA)—implanted in her visual cortex in an attempt to generate images depicting the world outside.
She didn’t hesitate to say yes.
Helping Blind People in the Future
Gomez always loved science as a child and in school. During her college years, she enjoyed biochemistry and decided to teach. She had been teaching high school biology for 15 years when she lost her eyesight.
She had just renewed her driver’s license that January before she quickly developed toxic optic neuropathy, a condition that rapidly destroys the optic nerves connecting the eyes to the brain. Within a matter of days, Gomez had completely lost her vision and any perception of light.
"It was a new year," said Gomez, "and just like that, it was a new life for me."

She spent months reassuring her sons, then ages 9 and 16, and learning to live with her new reality. Working with the National Organization of Spanish Blind People, Gomez learned how to be as independent as she could be. The organization taught her everything from how to locate food on a plate and shop at the supermarket to how smartphones and computers could assist in everyday life.
Her husband, Jose Luis, was already doing his part to help with household chores and the children, but now his role as her partner became even more essential. His support over their 33 years of marriage has made everything work. At home, she is not a blind person—just Berna.
When she spoke with Fernandez about the prosthesis experiments, she had accepted her new life.
"I know I am blind, that I will always be blind," she said. "But I felt like I could do something to help people in the future. I still feel that way."
How the Experiments Worked to Create Artificial Vision
During a three-hour surgery, a neurosurgical team needed only about a minute to implant the tiny microelectrode array, much smaller than a penny, into the visual region of her brain. The procedure went as expected, without complications.
For the next six months, Gomez spent up to four hours each day in the lab with Fernandez and his team conducting experiments that yielded important data. It wasn’t easy.
After sighted people go blind, they can still experience spontaneous phosphenes. Over time, these disappear. But Gomez’s surgery induced new spontaneous phosphenes to occur. While these decreased over time, she had to learn to distinguish a naturally occurring phosphene from one evoked by electrical stimulation via the array. That process alone took two full months. The work was methodical as researchers asked Gomez to describe what she perceived and even rate the brightness of each phosphene.
The experiments ultimately determined the amount of electrical current that could safely be used to produce phosphenes. The team also confirmed the biocompatibility of the equipment used in the prosthesis.
In addition to identifying lines, Gomez also described seeing a large and small "O." She even brought one large and one small sequin to the lab from home to explain the images. To get Gomez more familiar with evoked phosphenes and to introduce variety, lab members created a video game for her to play: a simple black-and-white maze that she moved a circle through using visual images created with the prosthesis.
While a neurosurgeon placed just one array in Gomez’s brain, published research conducted by Normann indicates between seven and ten arrays in the visual cortex, working together, could produce more detailed images for useful vision.
"This could give a blind person more mobility," said Normann. "It could allow them to identify a person, doorways, or cars easily. It could increase independence and safety. That’s what we’re working toward."
What the Future Holds for Artificial Vision
The work to get to this point has been painstaking.
"When we started this project more than 30 years ago, there was nobody doing anything in this field, and we needed so much basic information," said Normann.
After developing the UEA in the 1990s and unique tools required to implant it, Normann conducted years of experiments to answer key questions in the quest for artificial vision. The result is a foundational body of work encompassing more than 100 published papers, cited by scientists around the world.

"I would like to have something like this prosthesis, even if it were very simple. As a blind person you don’t know where a door is, or a window, or a person. With this you would at least know something was there."
Berna Gomez
Normann will now work with Fernandez to conduct similar experiments with as many as four other patients in Spain before beginning additional research efforts in the United States. The next set of experiments will use a more sophisticated encoder system, capable of stimulating more electrodes simultaneously to reproduce more complex visual images.
For Moran CEO Randall J Olson, MD, work on the Moran | Cortivis Prosthesis heralds a remarkable leap forward for the field.
"The results are amazing, and I couldn’t be more excited about the possibilities for the prosthesis," said Olson. "For years, Dick and his collaborators have been pushing the boundaries of what people believed to be possible. Their dedication has paid off spectacularly."
The most recent advances with the prosthesis wouldn’t have been possible without Gomez, who says she’ll always answer the call to help in whatever way she can. Surgeons removed the array from Gomez’s brain at the end of the experiments, but she remains a key member of the team, currently assisting by speaking with potential new prosthesis study participants who may have questions or concerns.
She doesn’t feel especially brave, only clear about her decision to participate in the research and the useful feeling she has derived from it.
After thinking about it for a moment, Gomez says: "Someone has to do it."
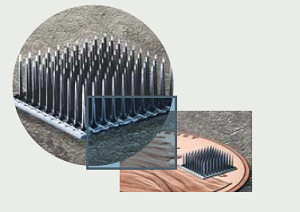
About the Utah Electrode Array (UEA)
Invented by Richard "Dick" Normann, PhD, the UEA is only 4mm by 4 mm.
It has one hundred 1.5-mm-long microelectrodes that can both record and replay the electrical activities of neurons communicating in the brain.
Normann first used the array in amputees to evaluate safety and efficacy, and it has allowed the amputees to control artificial limbs simply with their desire to move a finger or hand. In Spain, a team led by Normann and Eduardo Fernandez, MD, PhD, implanted the UEA into the brain’s visual cortex for the first time.