THE RIPPLE EFFECT

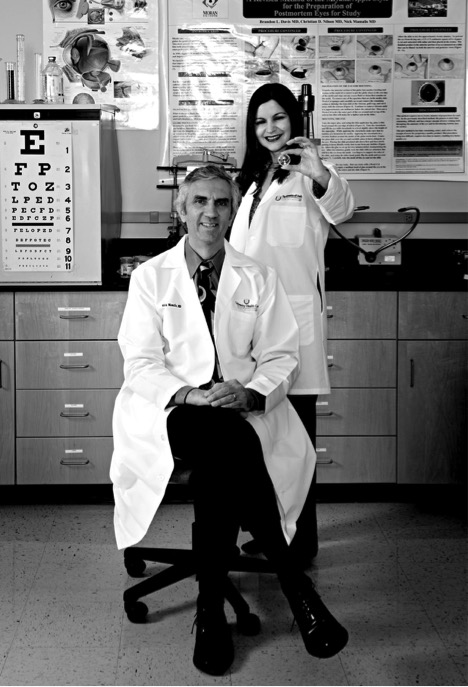
Perched on the foothills overlooking the Salt Lake Valley, Moran's Intermountain Ocular Research Center sits at the crossroads of global research, education, and patient care. At its helm, Nick Mamalis, MD, and Liliana Werner, MD, PhD, have revolutionized intraocular lens (IOL) implants, design, and surgical techniques. They advise and educate a worldwide network of ophthalmic surgeons, clinical researchers, and intraocular lens designers. And every day, everything they do ripples out into the community by helping to restore vision to millions of patients.
To fully understand the impact that Mamalis and Werner have on cataract surgery outcomes, consider this: last year, over 6 million people throughout the world received intraocular lens implants during cataract surgery the most commonly performed surgery today and practically every one of those lenses or prototypes was tested by the Mamalis Werner lab.
Pioneers
For the past 30 years, Moran's Intermountain Ocular Research Center has emerged as the go-to center for new IOL technologies and design, for IOL-related complications, for surgically removed IOLs, and for ocular tissue with lens-induced disease. "There are very few labs in the entire world doing the kind of work we do," says Mamalis. "When we began in the early 1980s, there were no centers doing any IOL analysis or research we were the pioneers, and today we are doing the ultimate in translational research. As a surgeon, what excites me the most is actually being able to take an implant in the very early design phases, work to make it a better implant, get it approved, and put it in my patient's eyes."
Combined Experience
Lens manufacturers partner with the Intermountain Ocular Research Center because of the team's combined expertise: both Mamalis and Werner specialize in lens design, materials, and surface modifications, such as the shape and size of the optics the part of the lens that focuses on the retina and the haptics small filaments connected to the optics that hold the lens in place in the eye. Also, they look at how these materials interact with ocular tissue.
Master Sleuths

Despite the technological advances in cataract surgery, challenges of all kinds present themselves. Lens design flaws not to mention the occasional baffling mystery find their way to the Mamalis Werner lab. "While surgically removing an implant is relatively uncommon less than one percent the impact is still huge," says Werner. "Since 2000, our lab has received over 8000 explanted IOLs from all over the world needing to be evaluated for flaws or complications; some very puzzling." The team examines the history of each lens, identifies flaws and successes, and prepares a report for every lens. Findings help doctors around the world make better surgical and lens choices for each of their patients and help lens manufacturers improve their designs.
Never, Ever Routine
The center also functions as a registry for removed IOLs and eye tissue with lens-induced disease. Packages arrive each week malfunctioning lenses from manufacturers, calcified lenses, opacified lenses even actual donated eyes with lenses still in them. "We honestly don't always know what the day will bring. I may get a lens that is so interesting, I want to stop everything and dedicate myself to that. It is so exciting," says Werner. "One day, we received a box with various explanted IOLs that had mysteriously turned white. Scrupulous detective work led us to discover that the lenses had been stored near pesticides and had absorbed some of the chemicals. Another day, a surgeon from Brazil actually flew to Moran with an explanted corneal implant in her carry-on luggage for me to evaluate. Our work is never, ever routine. I think if I improve anything from developing future lenses to figuring out a problem it doesn't just impact one patient, but so many people, including manufacturers and ophthalmologists. If we can change one surgeon's thinking, we have helped all of his patients. I'm very proud of that."
TASS Task Force
Cataract surgery is one of the safest surgeries performed today, but some post-operative complications can occur. One day, in the late 1980s, Dr. Randall J Olson, chairman of the Moran Eye Center received a call from a baffled and concerned doctor who said all of his Friday cataract patients developed tremendous inflammation after surgery, and he wasn't sure why. Dr. Olson immediately contacted Dr. Mamalis, and upon investigating the matter, they discovered a heat-resistant toxin in the ultrasound bath in which the instruments soaked during the week. By Friday, this bacterial toxin formed on the instruments causing patients' raging post-surgery eye inflammation. As a result of this finding, the American Society of Cataract and Refractive Surgery (ASCRS) asked the lab to help evaluate unexplained inflammatory complications following cataract surgery. So they developed the Toxic Anterior Segment Syndrome (TASS) task force. The task force gets calls from surgeons worldwide asking for help with cases of post-op inflammation, 80 percent of which, to this day, are caused by problems with instrument cleaning and sterilization.
Ripple Effect
"As a physician, one of our primary goals is to give patients the best possible vision and to prevent vision loss. This is why we go into ophthalmology. There is extensive research in blinding eye diseases like macular degeneration and other diseases of the retina, but we don't want to forget that we also want to treat preventable blindness, and that's where our research comes in cataracts are a tremendous cause of preventable blindness," says Mamalis. "We can better our surgical techniques and better the implants that go into providing the best possible vision for our patients' eyes. But we could not have been doing the work we do in a different setting. Moran is really unique for a major research institution, and it all starts with Dr. Randall Olson. He gives us the necessary resources and allows us the independence and latitude to do the work that we see fit. It is amazing."
The Next Big Thing
Corrective cataract lenses have developed from a single distance-only monofocal lens, to a multifocal, which corrects vision for near and far, eliminating the need for glasses. The bulk of what the lab is working on now is designing a truly accom¬modating implant that will give patients clear, near, intermediate, and distance vision without compromising their vision or breaking up the light as it comes in. There are also designs for implants that actually have separate optics that come together and go apart to allow people to see both near and distance clearly. In addition, the lab is work¬ing on a lens with silicone oil inside its haptics. The silicone moves to the center of the lens when the patient focuses up close, changing the curva¬ture of the lens and providing near vision. When the patient focuses far away, the silicone moves to the periphery of the lens where it won't affect the curvature of the lens, similar to the way the normal human lens works. And they are working on a lens that can have its corrective power modified by an exchangeable optic or even changed by a laser, designed for a child, for example, whose eyesight changes as he or she grows.
Cataract Surgery Then and Now
From post-World War II through the 1970s, cataract surgery required removing the natural lens by making a large incision, removing the cataract in one piece, and applying multiple sutures. Patients suffered a lengthy recovery, and after it all, still had to wear thick "Coke bottle" glasses.
Since the 1980s, cataract surgery has improved markedly. Sophisticated intraocular lenses are now placed directly in the eye after a cataract is removed, allowing people to have functional vision without having to wear thick glasses. Implants were originally made of a stiff Plexiglas-like material. Now, we have foldable lenses that can go into the eye through a miniscule incision that doesn't require sutures. Surgical techniques have improved as well, from removing cataracts manually to using ultrasound and lasers. All of these improvements allow the patient to rapidly go back to normal activity, often the day after surgery.