Episode Transcript
Announcer: Medical news and research from University of Utah physicians and specialists you can use for a happier and healthier life. You're listening to The Scope.
Interviewer: Every house has different things around in case there is an emergency. Like you might have a first aid kit, a fire extinguisher, maybe even an EpiPen if you have somebody with allergies. There's one more thing you should add to that list. It's called a naloxone kit. Dr. Jennifer Plumb is one of the founders of UtahNaloxone.org. You're also in pediatric emergency medicine. So I was wondering if you could start with a story, perhaps, about having a naloxone kit in your house could change the outcome of an otherwise tragic situation.
Dr. Plumb: We see all kinds of scenarios of children overdosed on opioid medications as well as narcotics. One that comes to mind of a grandparent who was being treated for cancer on a chemotherapy regiment and also needed pain medications. And the grandchild, unfortunately, got a hold of one of the pills and overdosed on it.
Just as an example of how frequently these are seen, I personally saw a four-week period with four children on my shifts who came in overdosed on medications that they came into contact with either in their home or in the home of somebody else. And those were all kids under the age of eight. The reality of it is as just about any scenario that you can think of that a kid can get into trouble with a medication, they can get into with opiates. And unlike other medications that they can get into and take, these medications can kill them. One pill can actually kill them.
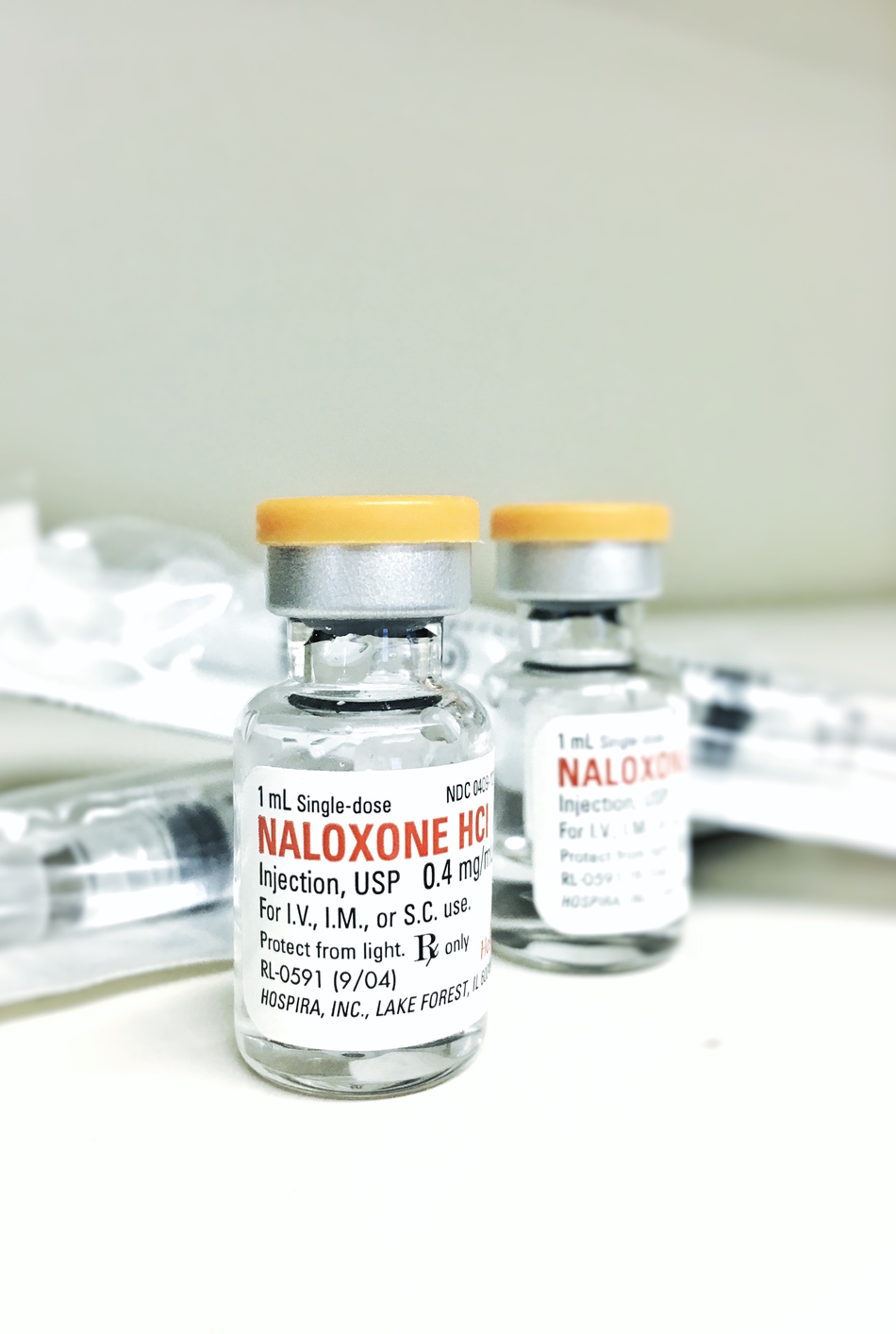
Interviewer: So let's back up for a bit here. naloxone, what exactly is it?
Dr. Plumb: So naloxone is an antidote. It's a very pure substance. All it does is reverse an opiate overdose. It doesn't relieve pain, it doesn't get someone high, it's not addictive, you can't overdose on it. So it is just purely an antidote to opioids. So what are opioids? Opioids are OxyContin. The medication in that is actually oxycodone. You can also see that in Percocet and other medication. It's methadone, it's morphine, it's fentanyl, it's codeine. These are medications that we've all periodically had in our homes after surgical procedures or traumas. It also is an antidote for heroin and all of those substances are very, very similar biochemically. Very, very similar.
Interviewer: So get a little geeky for me here. How does it work exactly? So what causes an opioid overdose and then how does naloxone reverse that?
Dr. Plumb: Absolutely. We know you physician types like that nerdy stuff.
Interviewer: And I like hearing these types of stories because it fascinates me.
Dr. Plumb: And it is really simple. I think of receptors in the brain as like a golf tee. They have a little cup and you have substances that trigger those receptors. We have all different kinds of receptors in our brain. A receptor that's triggered by opiate medications or opioid medications is exactly that, an opiate receptor. So if you picture the opioid coming to sit on that tee like a golf ball, it gets on there, it does what it's supposed to do. It relieves pain, provides analgesia, provides comfort.
Unfortunately, if too many of those receptors are filled by the opiate medication, it causes an overdose. And an overdose of an opiate medication causes respiratory depression. So when you overdose on one of these substances you stop breathing. They look blue or gray if they're darker skinned because they're not getting oxygen. They're not breathing. They also get these really tiny pupils, almost looks just like a fleck of pepper. So these are the things we tell people to look for when they overdose or when they see someone they think is overdosed and that is the cue. "Holy moly, we need to call 911. We need to get naloxone into this person."
Traditionally, paramedics, EMTs, ER doctors were the only ones that could provide that antidote. Fortunately, it's now legal for people to have in their home so that if they find someone overdosed, they can start the reversal of the overdose before the EMS personnel even arrive. We always tell folks, "Call 911. Give them naloxone." And that way, hopefully, ideally, by the time EMS is there, your loved one's breathing again and you've bought those extra minutes that are so important and so crucial of oxygen to the brain.
Interviewer: So you say it's legal for now for anybody to own. What changed?
Dr. Plumb: In 2014, a bill was passed here that made it legal for a physician to prescribe naloxone to anyone. And this is unique. Anyone who's either at risk of an opioid overdose or at risk of witnessing an overdose. So traditionally, if I write you a prescription, I write it for you. It also made it legal that it could be prescribed without a physician-patient relationship, which is unique.
Normally, I have to have a relationship with you, as a patient, if I'm giving you a medication. Well, in this case, if I have, say, a 16-year-old who overdosed on heroin and their parents are desperate to have coverage in the home just in case, I can absolutely write a prescription to that mom, to that dad, to that significant other. And that's unique in the law, but it's very important that it's in the law.
Interviewer: Is it dangerous on its own?
Dr. Plumb: Absolutely not.
Interviewer: No danger to have it in the home?
Dr. Plumb: No. If I gave it to you right now you would feel the little prickle from the injection. You would have no effect from it whatsoever. You can't overdose on it. We have people sometimes say, "Well, what if it's not an overdose and I give them the naloxone? What if?" And the reality of it is if you had a heart attack, if you're having a stroke, if you've had a brain injury, if it's related to a diabetes problem, it won't do a thing. It won't hurt them, it won't help them, but when your EMS providers get there because you've called 911, they're going to also know this person that's down didn't respond to that Narcan. We need to start thinking about other things as well as the additional medical care. So it really is about as safe as any medication that we know of out there.
Interviewer: There are a lot of resources. Is it Utahnaloxon.org?
Dr. Plumb: It is.
Interviewer: I've noticed you have all sorts of resources on how to use it, what's going on when you use it, where to get it. Do you have any final thoughts as we wrap up this conversation?
Dr. Plumb: I think that the thing I would really like to get into people's heads is that this epidemic, and it really is an epidemic, the CDC has called the crisis we're having in this country with opioid overdose as an epidemic, is it's really okay to talk about. It's really okay to think about. It's really okay to look at what's going on in your own personal home and say, "You know what? We don't really want to tell people about this, but we need to be prepared and we need to be willing to have this conversation."
Have the conversation with your physician. Have that conversation with your therapists. Have the conversation with people who are involved in your healthcare. If you're not getting anywhere with that, have the conversation with us. We can be called 24/7 and we can get naloxone into people's homes. It's just more important to us that lives are saved. These are unnecessary losses of life.
Announcer: TheScopeRadio.com is University of Utah Health Sciences Radio. If you liked what you heard be sure to get our latest content by following us on Facebook. Just click on the Facebook icon at TheScopeRadio.com.