Episode Transcript
Dr. Miller: You've been told that you might need a Whipple. What does that mean? We're going to talk about that next on Scope Radio.
Announcer: Access to our experts with in-depth information about the biggest health issues facing you today. The Specialists, with Dr. Tom Miller, is on The Scope.
Dr. Miller: Hi, here with Dr. Courtney Scaife. She is a professor of surgery here in the Department of Surgery at the University of Utah. And she also specializes in cancer surgery. Courtney, what is a Whipple?
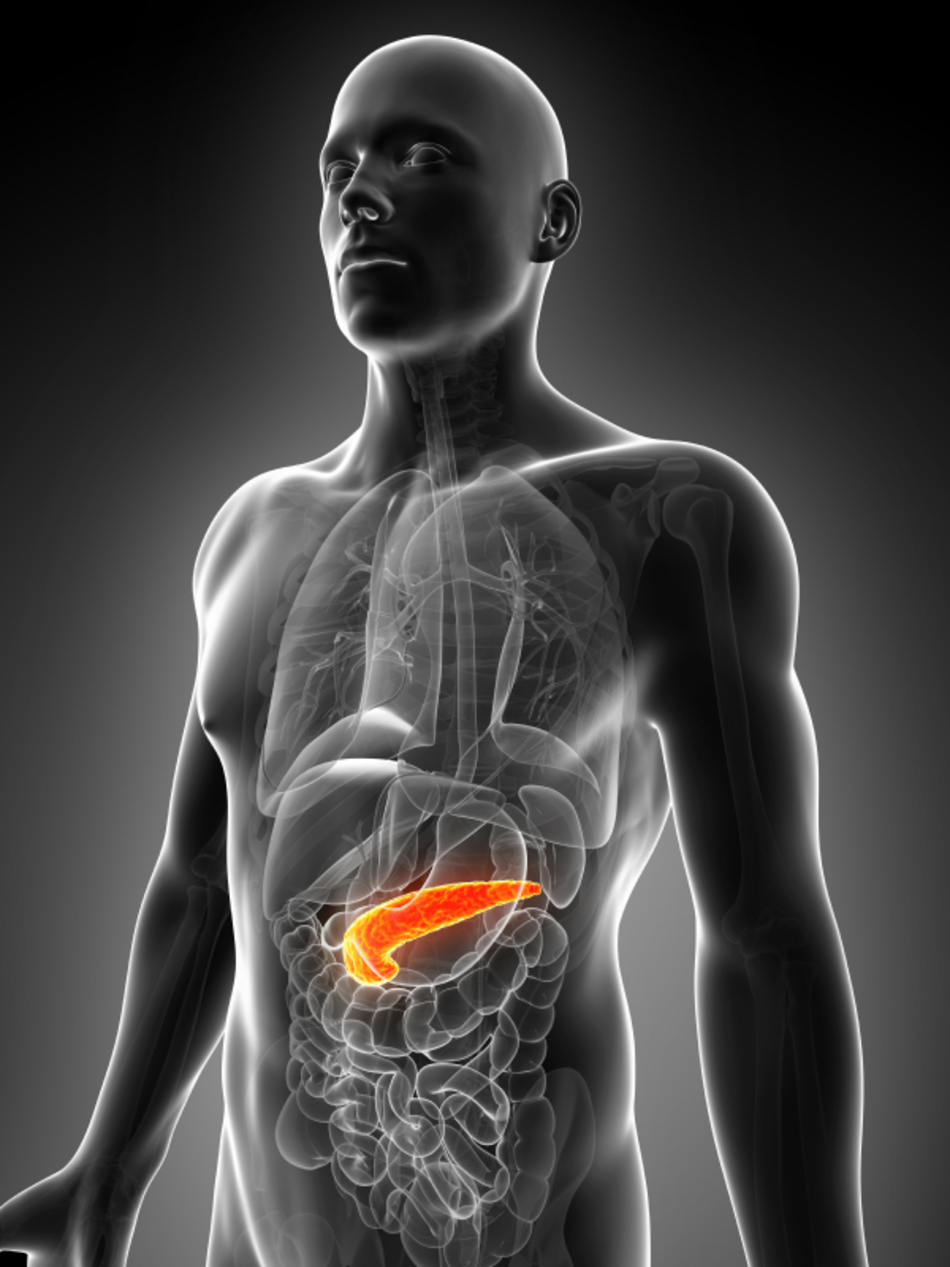
Dr. Scaife: A Whipple is an operation on the pancreas when you have a neoplasm, which can be a mass or a tumor or a cyst, those are all synonyms, in the proximal part or we call it the head of your pancreas. And the Whipple removes that part of the pancreas.
Dr. Miller: So the Whipple is the name of the type of surgery that you do. Is that pretty typical as pancreatic surgery goes?
Dr. Scaife: That's correct. Well, the Whipple is the only surgical procedure of the pancreas that's named after the doctor who first described the operation. Other pancreas surgeons are often more anatomically referenced, such as a distal pancreatectomy or an enucleation of a tumor out of the pancreas.
Dr. Miller: So Whipple has been a surgery that's been practiced for many years, I think. Is that right?
Dr. Scaife: Dr. Whipple first described the operation in the 1950s. And as first described, it was a two-day operation where the pancreas was taken apart, and the next day, everything was put back together.
Dr. Miller: My understanding is that Whipple surgery is a curative surgery for some patients with pancreatic cancer.
Dr. Scaife: That's correct. So again, Whipples are done for all types of neoplasms. And again, neoplasms can be masses, tumors, cysts in the pancreas. And so a Whipple for a non-cancerous neoplasm is obviously curative. And a Whipple for pancreas cancer can also be curative.
Dr. Miller: If one has a pancreas cancer and they're going to undergo Whipple, the purpose of that would be to cure the cancer, I think, obviously, right?
Dr. Scaife: Yes.
Dr. Miller: And once that takes place, what can the patient expect after a Whipple surgery?
Dr. Scaife: So a Whipple operation is complex. It's a six- to eight-hour operation.
Dr. Miller: That's a big operation.
Dr. Scaife: Yeah. And because of the location of the head of the pancreas intimately involved with the bile duct and the first part of the small intestine, we have to rebuild all of those. So we rebuild the pancreas. We rebuild the first part of the small intestine. And we rebuild the bile duct. But in the end, the patients can eat normally. They can eat any food they like. And they do quite well after recovering from the operation.
Dr. Miller: Is there anything that you tell your patients in that preoperative period when you first meet them before they undergo the surgery?
Dr. Scaife: We frequently tell patients that the surgery, again, takes six to eight hours. They'll be in the hospital for approximately seven days. For a month after a big surgery like this, their appetite, their energy, and their strength will all be much lower than they normally expect. And it usually recovers four to six weeks after surgery.
Anything someone has before surgery gets a little bit worse and harder to manage after surgery. So diabetes, high blood pressure are all a little bit harder to manage after a big operation like this. But it recovers about a week or two after surgery and goes back to their baseline.
Dr. Miller: So that's interesting. Do you use a team approach with another physician such as an internist to help manage the patient after the surgery if they have diabetes or other complications?
Dr. Scaife: Generally we manage it on our own. Because they're short-lived, we're able to manage it on our own.
Dr. Miller: Do they ever experience diarrhea following pancreatic surgery? Is that something that they need to worry about?
Dr. Scaife: Yeah, chronic diarrhea after a Whipple operation is extremely uncommon, but not zero. Some patients get dumping syndrome, which happens in less than 10% of our patients.
Dr. Miller: What is that? What's dumping syndrome?
Dr. Scaife: It's from operating on the stomach and re-plumbing it effectively to the small intestine or rebuilding that first part of the small intestine. Some patients can have a syndrome where they eat rich foods, and the foods go through the stomach. And the next part of the small intestine, it's not used to seeing such rich foods, reacts by pouring a lot of water into the intestine.
And that neurologic response can result in almost like a hot flash-type symptom. And then after all of that water gets emptied into the intestine, 30 to 60 minutes after a meal, patients can have diarrhea from the water flushing through their system.
Dr. Miller: Now, generally, that resolves in a couple of weeks? Or does that continue?
Dr. Scaife: In 10% of our patients, after the Whipple surgery, they experience that. Fewer than 1% of the patients have a long-term problem with that. It normally resolves on its own and the few patients that it doesn't, learn to eat around it so they don't stimulate those symptoms.
Dr. Miller: So over time, people who have a Whipple procedure, they potentially are cured of their cancer. Do they end up keeping the same weight that they had before? Do they lose weight after a Whipple where part of the pancreas is taken out? And as I understand it, the pancreas is very important in digestion.
Dr. Scaife: That's right. So the answer to the first part of your question is that most of our patients, 80% of our patients, do well and maintain their normal appetite, normal diet, and normal weight. We do have different ends of the spectrum, obviously. There are some people who gain weight and some people who don't eat as well after the operation, but that's very unusual.
The second part of your question, the pancreas does two things. It manages your blood sugars and it helps you with digestion. And so after we remove part of the pancreas, it's very uncommon to cause someone to be a diabetic from a pancreas surgery. You only need 10% of a normal pancreas to manage your blood sugars normally. So very few people become diabetic as a result of the operation.
Dr. Miller: So you're not taking out the entire pancreas during the Whipple.
Dr. Scaife: Correct, correct. And really about a third to only 20% of the pancreas comes out with the operation.
Dr. Miller: Now, this is a big operation, as you've outlined. Do patients experience much pain postoperatively or in the several months following surgery?
Dr. Scaife: No, we're really able to manage the pain very well. We use local anesthesia in the incision or an epidural in the postoperative care. And then patients actually recover quite well in usually one to two weeks out from surgery. They're off of any pain medications and starting to resume their normal activities and functions.
Dr. Miller: Can you give us a wrap-up about who comes to you for potential surgery?
Dr. Scaife: Most of our consults for pancreas neoplasms are simple cysts or benign cysts in the pancreas. And so 80% of our patients don't need an operation, even though they're referred to us for evaluation. Of the few that do need an operation, those patients do extremely well. They don't all need Whipples. There are other less invasive operations of the pancreas that can be done. And all of those patients, including the patients who do Whipples, ultimately return to a very normal lifestyle.
Announcer: TheScopeRadio.com is University of Utah Health Sciences Radio. If you like what you heard, be sure to get our latest content by following us on Facebook. Just click on the Facebook icon at TheScopeRadio.com.