Interviewer: You have pretty severe stress urinary incontinence, and it's been recommended you consider a surgically implanted device called an artificial urinary sphincter.
Urologic surgeon, Dr. Benjamin McCormick at University of Utah Health is an expert in male urinary incontinence, and today he's going to help provide us with what men should know when making this important treatment decision.
What Is an Artificial Urinary Sphincter (AUS)?
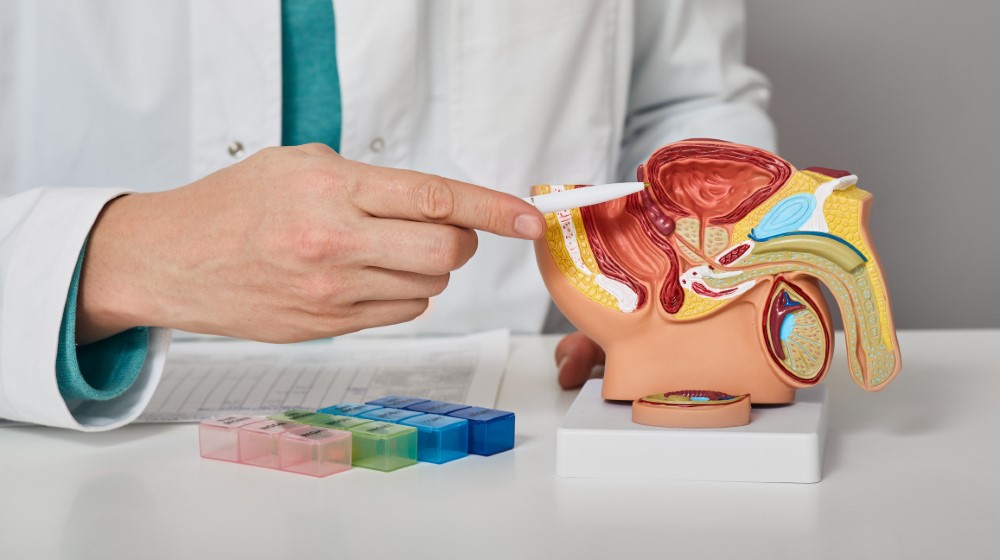
Dr. McCormick: It's a mechanical device. It comes in three parts that are all connected. The first part is a saline-filled cuff that surrounds the urethra. The urethra is the pee channel that your pee comes out of. The second part is a balloon that applies pressure to that cuff, and that balloon is situated in the abdomen. And then lastly, there's a pump that pumps the fluid from the cuff to the balloon when you're ready to pee, and that is in the scrotum.
AUS for Treating Stress Urinary Incontinence
Dr. McCormick: We typically quote patients that they can expect an 80% improvement wherever they are. And so if someone's floridly incontinent, they have no control, then, they're wearing, 4, 5, upwards of 10 diapers a day, they can expect to be at 80%, which could mean 3, 4 pads a day. And so it's not going to be . . . I would never counsel anyone that they would be dry, completely dry in every scenario after this procedure. And so it's important to manage expectations. It's also difficult to make a huge difference in someone's life when they're at zero than when they're at say 95% and they leak very rarely, but it's still bothersome. Not to say that those patients wouldn't be a candidate for a procedure, but that it's easier to make someone happy going from 0 to 80 than it is from 95 to 97 or 98.
Interviewer: Sure. So about an 80% improvement rate from wherever the individual is . . .
Dr. McCormick: Right.
Interviewer: . . . you would define that kind of in the usage of how many pads you might use in a day. But what about the actual stress that causes those things to happen?
Dr. McCormick: Yeah. For example, standing up from a chair, swinging a golf club, or lifting something heavy. Sure. It's really dependent on the person, but we see that all the time.
Interviewer: And then what about the satisfaction levels?
Dr. McCormick: Yeah, very high.
Interviewer: You're getting some pretty satisfied patients?
Dr. McCormick: Yeah, 90%, 95% of patients are satisfied, and would have it over again.
Interviewer: And when they tell you, "Yeah, I'm really satisfied," what are the reasons they give for that?
Dr. McCormick: They can do things again that they've not been able to for a long time. They can go to Six Flags with their grandkids and not have to worry about changing their pads every hour or something like that. I think that's pretty common. Play golf, not have to worry about putting pads in their bag or what have you. So I think things like that. Also, pads, pull-ups, diapers are expensive, and so reducing that cost, I think is not insignificant.
Interviewer: What are some of the common questions that men have when it comes to this particular procedure?
Dr. McCormick: They're worried about pain, which is usually transient. Not a whole lot of pain with the procedure usually, but anytime you make an incision, there's a low but non-zero risk of chronic pain. I've not seen that personally, but I certainly have heard of it. And then, using the device does take some learning and adjusting. I mean, every time you stand over a toilet, you've got to press this button in your scrotum. So that takes some getting used to, and there's some anxiety around that. The life span of the device, is, generally, thought to be about 8, 10 years, sometimes more, or sometimes less. It's just a mechanical device and so it has moving parts that can fail. And so if that's the case, we just kind of take it out and replace it. Usually not a big problem. So I think those are the main points that patients hit me with.
Recovery and Activity Restrictions After AUS Implantation
Interviewer: Yeah. And when you talk about recovery time being about six weeks, does that mean six weeks of no working and no activity? Or what does that look like, that part of the recovery?
Dr. McCormick: Yeah. Good question. We send patients home the same day usually, unless there's some extenuating circumstance, often without a catheter. And the next day they can walk, climb stairs, shower. But, yeah, would like them to refrain from doing heavy lifting, 15, or 20 pounds for 4 to 6 weeks, deep squats, or things like that. Certainly not riding a bicycle for a good two, or three months.
Interviewer: Sure.
Dr. McCormick: But otherwise, I think patients relatively quickly return to their normal lives.
Interviewer: And is this device pretty durable? Like after I heal, can I go back to doing the things I want to do, like golf, or if I'm a runner, I can go back to running, or . . .
Dr. McCormick: Oh, yeah. Yeah, absolutely.
Resuming Physical Activities
Interviewer: Physical activity at that point, is that not an issue at all?
Dr. McCormick: Yeah, no real restrictions after three months. I think certainly patients can listen to their bodies and kind of start picking up activity within the first couple of weeks. And then I just don't love when people are on bicycles or horses, especially, kind of within three months, I think it's pretty delicate. But after that, yeah, no problem.
Impact on Intimacy and Sexual Function
Interviewer: What about intimacy and sexual function? Are men concerned about that? And then, like, what impact does this device have on those two things?
Dr. McCormick: Yeah, for sure. Definitely, men are interested, to say the least.
Interviewer: Sure. Right?
Dr. McCormick: I think by and large this procedure helps a ton. What I'll say in my experience is that it's really hard for men to get in the mood when they're leaking urine or if they have an erection and they're trying to be intimate, and they're leaking urine. I think that it's really tough, and that is the main reason that men come and see me about this. So in my experience, men who are having sex or able to have sex before this procedure are much happier, just because they're drier and they can be intimate with their partner and not have to worry about leaking as much.
Is an AUS Implantation Right for You?
Interviewer: What are some critical points of conversation or discussion that a man should have with their provider before actually making this decision? Are there some things that they really just need to . . . questions they need to have answered or things they need to have worked out?
Dr. McCormick: What I tell all patients really who, either my patients or friends or family who are seeking treatment, I think that asking a surgeon their outcomes and particularly their volume is really important. If a surgeon is doing kind of one of these a year, it's not ideal. I mean, this is a pretty complex surgery. It can come with its fair share of complications, and you really want someone who has experience in this.
Interviewer: Yeah. What's the minimum that you should look for then?
Dr. McCormick: I don't know.
Interviewer: How many procedures a year?
Dr. McCormick: I mean, I think the minimum would be something like five. I think a surgeon who does 5 a year is in the top 5% of implanters, I mean, I think that would be the absolute minimum. Ideally, double digits, a couple of dozen. And I think, importantly, is being comfortable. I never want to talk anybody into surgery. I think that's a recipe for disaster. I think that it's important that you have an honest and thorough conversation with your surgeon about your goals and expectations, their experience, and alternatives.
Non-Surgical Alternatives for Managing Urinary Incontinence
Interviewer: And what are those alternatives that patients should be aware of?
Dr. McCormick: I think that non-operative management can be a good answer for many men. Often we see patients who've undergone prostate cancer surgery have leakage. One of the mainstays of treating incontinence, especially in the early stage, is pelvic floor physical therapy. And I'm a believer that essentially everyone should see a pelvic floor physical therapist. I think they really are miracle workers. The pelvic floor physical therapist can be a real ally in helping these folks kind of regain some continence. It doesn't always work, but it's certainly something that should be tried before any of these surgical treatments.
Interviewer: What are some other non-surgical options that men try?
Dr. McCormick: So beyond pads and pull-up diapers type things, there are these devices called Cunningham Clamps, which can . . . it's basically a soft clamp that you place on the penis, that kind of holds the urine in. And so we have patients come in with those not infrequently. The problem is that they're not super comfortable. They don't necessarily work very well, and importantly they can cause pressure sores on the penis. And I've seen some pretty terrible injuries from Cunningham Clamps over the years. And I think they have their place for some men. However, I don't think that it's a good long-term option.
Yeah, I mean, condom catheters are another thing I see people use. Basically, it's essentially a condom that has a drainage tube at the tip, and it just kind of drains the urine into a bag that's on the leg. So that's another thing, but again, can cause irritation on the penis. And some men don't . . . I think they're uncomfortable. And so not a whole lot of great options, to be honest.
Deciding Between Surgical vs Non-Surgical Options for Managing Urinary Incontinence
Interviewer: When a man does decide on an AUS versus trying some of the other things, what are the deciding factors for them? Why this procedure?
Dr. McCormick: Well, for the right candidate, this procedure is the gold standard for moderate to severe urinary incontinence, and it can really change lives. I think that while I'll never try to talk anybody into surgery, if I think someone is a good candidate and they could really benefit, I'll tell them. And so, while I don't want to talk anybody into anything, I also don't want people to live with incontinence that could be treated. So it's tricky... it's a tough balance. But I think that for the right guy, this is really great.
Overactive Bladder in Women: Symptoms, Treatments, and How to Take Back Control
If frequent bathroom trips disrupt your life, you are not alone. Women's health expert Kirtly Jones, MD, talks to urogynecologist Whitney Hendrickson, MD...


