
Types of VADs, Total Artificial Hearts, & Other MCS
Information Regarding HeartWare™ LVAD
Medtronic is no longer making the HeartWare™ LVAD due to some health concerns. Please read the attached letter for specific information. Patient Information RE HeartWare LVAD
Ventricular Assist Device Types
All LVADs have three parts:
- a blood pump
- a computer, called a controller, and
- a power supply that remains outside of the body.
This equipment connects to the LVAD via a series of wires. The series of wires is called a driveline.
University of Utah Health’s Mechanical Circulatory Support Program uses the most advanced and reliable ventricular assist devices (VADs) available for patients . Features of each LVAD may be different depending on the manufacturer. Talk to your clinician about which LVAD might be right for you.
Note: An LVAD is a type of VAD. VADs can support the left ventricle (LVAD), the right ventricle (RVAD), or both (BiVAD). However, the LVAD is the only device that patients can leave the hospital with.
Left Ventricular Assist Devices (LVADs) & Total Artificial Heart (TAH)
HeartMate 3 LVAD
The HeartMate 3 is the newest type of LVAD that the FDA has approved. It is a small centrifugal pump that uses a fully magnetically rotor to reduce blood cell breakdown. (A levitated rotor means that the pump has magnets on all sides to lift the rotor off the floor of the pump. This way the rotor will never touch the side walls of the pump and destroys fewer red blood cells.)
Both Bridge to Transplant (BTT) therapy and Destination Therapy (DT) use the HeartMate 3.
Doctors implant the HeartMate 3 by surgery through the sternum (or chest). This is called a sternotomy. Or doctors may use a , which is a less invasive . (In a thoracotomy, doctors access your heart through an incision in the ribs.)
The HeartMate 3 has wires (a driveline) that come out of the body in the upper abdomen. The HeartMate II and HeartWare LVADs also have drivelines that extend outside the body.
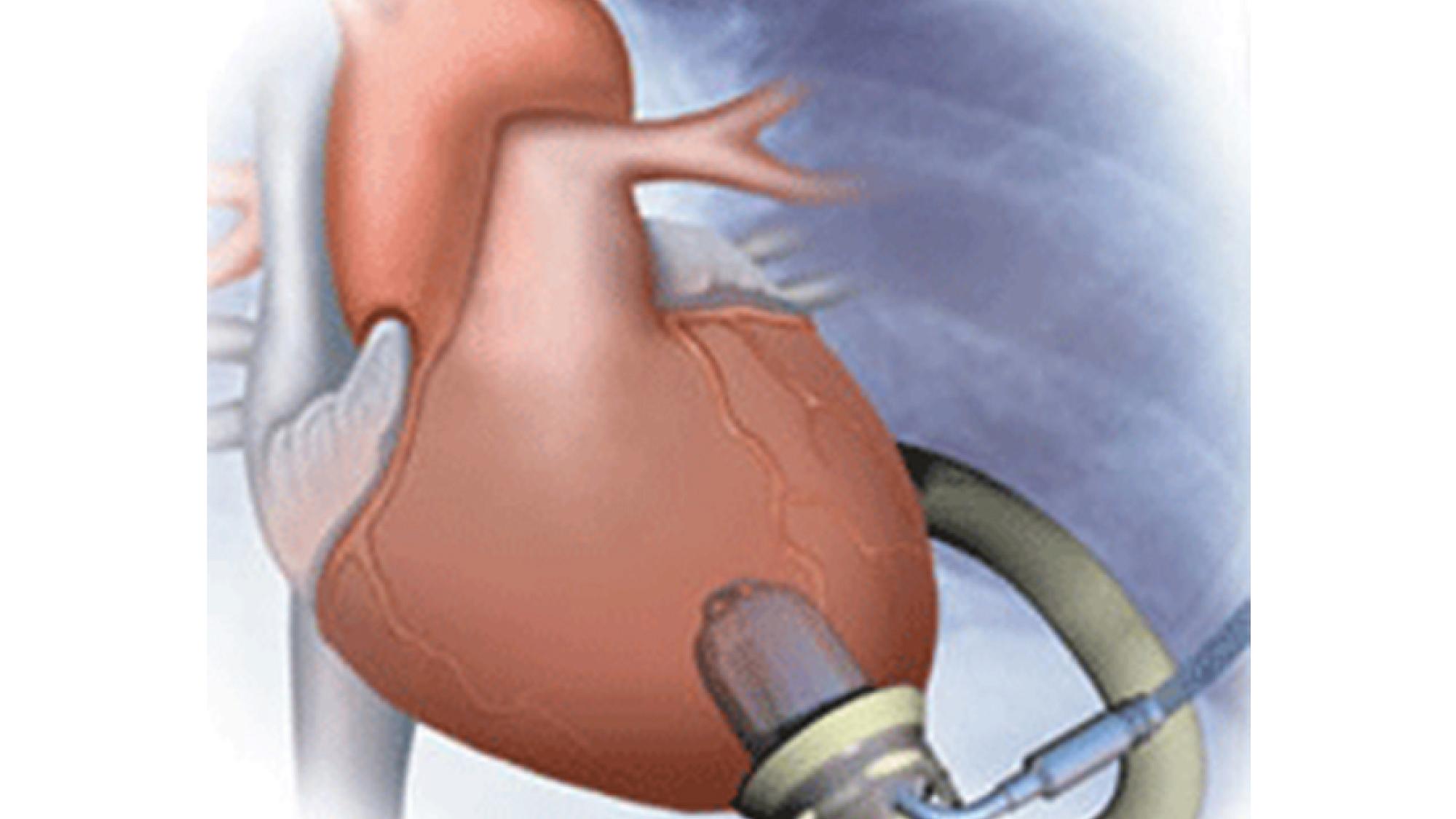
HeartWare (HVAD)
The HeartWare(TM) HVAD(TM) is a small centrifugal pump. Because of its size, doctors can implant it via a sternotomy or thoracotomy. It is also approved by the FDA as a Bridge to Transplant (BTT) therapy or Destination Therapy (DT).
The HeartWare sits in the area around the heart called the pericardial space. Like the other LVADs, the HVAD(TM) has a driveline (external wires) that come out of the body at the abdomen through a small surgical incision.
Heartmate II LVAD
The HeartMate II left ventricular assist system is an axial device. Because of its size and shape, doctors can implant the HeartMate II beneath the diaphragm.
It is FDA approved as both A Bridge to Transplant (BTT) therapy or Destination Therapy (DT). Public figures Vice President Dick Cheney and baseball legend Rod Carew both have the HeartMate II.
Jarvik 2000
The Jarvik 2000® LVAD is an axial flow pump that is currently in clinical trials. This pump has a few differences that set it apart from the other LVADs.
While all other LVADs have drivelines that leave your body through the abdomen, the Jarvik 2000® has a post-auricular cable. This is a cable that exits your body just behind the ear. Behind your ear, the cable attaches to your skull.
Having a cable behind your ear allows you to be more active around water, such as pools, hot tubs, and lakes. You can go under the water without worrying about your driveline incision getting infected. The Jarvik 2000® controller and batteries, however, are NOT waterproof.
This LVAD relies completely on battery power. There is no option for wall power. Additionally, you can change pump speed settings for this LVAD on the controller.
Axial Flow vs. Centrifugal Flow
Axial flow is a straight flow or parallel flow, whereas the HM3 and HW pumps are centrifugal or circular (radial and perpendicular) flow.
Total Artificial Heart (TAH)
Syncardia Total Artificial Heart
If both of the ventricles of your heart fail (left and right), a total artificial heart (TAH) is an option. We mainly use the Syncardia Total Artificial Heart for patients who are waiting for heart transplant. The TAH makes both ventricles and all four valves pump blood to the lungs and through the heart.
An external driver connects to the artificial heart by two tubes, called cannulae. The driver delivers pulses of air through the cannulae to inflate and deflate diaphragms in each ventricle. This action is what creates circulation from the TAH to the rest of the body.
If you have a TAH, you don’t have to remain in the hospital. You can return to daily life.
Other Temporary Mechanical Circulatory Support Therapies
Abiomed Impella
The is the world’s smallest heart pump. Currently the only percutaneous cardiac assist , (Percutaneous means that the doctors can insert the device through the skin.) Doctors implant an Impella through a transcatheter.
Specialists in the catheterization will insert the Impella devices into the left ventricle through the femoral artery into the ascending aorta, across the aortic valve, and into the left ventricle.
Different sizes of Impella can offer more or less support. Impella support is only temporary. You may have it only when we admit you to the hospital for a heart condition or symptoms.
ECMO
The extracorporeal membrane oxygenation (ECMO) is not technically a VAD. It is, however, another form of mechanical circulatory support therapy if you have severe acute respiratory and/or cardiac .
If you have had treatment, but that treatment has not been successful, specialists will consider giving you ECMO therapy. Doctors might consider ECMO if you have had cardiac arrest or heart failure. In this case your heart cannot pump enough blood to your organs. Sometimes specialists use ECMO therapy after heart surgery if the patient needs it.
ECMO is a technically complex procedure. It allows us to fully support your breathing and heart functions while your organs recover and/or you wait for a longer-lasting device.
Rotaflow, CentriMag, and CardioHelp
Rotaflow, CentriMag, and CardioHelp are external continuous flow devices. This means they sit outside the body and help your body circulate blood so that your organs don’t shut down. You may receive this if you have acute heart and/or lung failure.
Though these continuous flow devices are temporary, they will help stabilize your organs until we can get you a more long-term therapy option.
We Welcome Your Feedback
Questions or comments for the VAD team? Please email us at vadteam@hsc.utah.edu.
Meet Our Patients
Healing Through LVAD and Medication
Stavros Drakos, MD, University of Utah Health cardiologist, helps heal Anne Binger’s failing heart through use of an LVAD and medication.
Heart Failure Recovery After Pregnancy Via LVAD
Headed for heart failure after delivering her baby, Brenna was able to recover with an LVAD.



