Evaluating Male Fertility
Our ability to diagnose and treat fertility problems has greatly advanced over the last decade. Getting a complete and accurate diagnosis is essential to finding the best treatment or therapy for you.
Our andrology laboratory offers several diagnostic tests that can help your treatment process, including semen analysis, sperm penetration assay, and an anti-sperm antibody test.
Acrosome Stimulation Test
The acrosome cap is a structure inside the sperm head that surrounds the upper 40-60 percent of the sperm nucleus. The acrosome must work correctly for the sperm to penetrate the egg coating (or zona pellucida).
After the acrosome reaction, the sperm reveals binding sites that it needs to fuse to the egg. The acrosome stimulation test (which uses a double-detection system) identifies sperm that have acrosome reacted normally to artificial stimulation.
Anti-Sperm Antibody Test
All men have barriers that hide sperm from their body’s immune system. These barriers help keep your body from identifying your sperm as foreign, dangerous, and producing a defense against it. When these barriers break down, the body produces anti-sperm antibodies. If these antibodies attach themselves to sperm, they damage sperm’s ability to move and/or agglutinate (clump with other cells).
Women may also produce anti-sperm antibodies. We can test for antibodies by evaluating seminal fluid, semen, and the serum from the woman. You should have an anti-sperm antibody evaluation if:
- your sperm motility is low when you’re getting ready for a vasectomy reversal,
- you have a higher amount of agglutination,
- or if your sperm may not be working correctly.
Women should be tested for anti-sperm antibodies if a sperm cervical mucus interaction assay test suggests a problem.
Cervical Mucus Interaction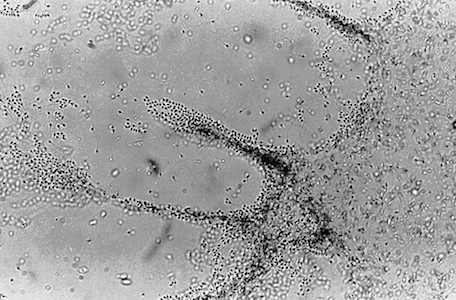
Next, we will record the motility of sperm that have penetrated the mucus every 30 minutes. If the donor sample performs better than the patient’s sperm, then the patient may have infertility. If both sperm samples don’t perform well, then the woman’s cervical mucus may be responding to the sperm in a hostile way.
Hamster Egg Penetration Test (Sperm Penetration Assay)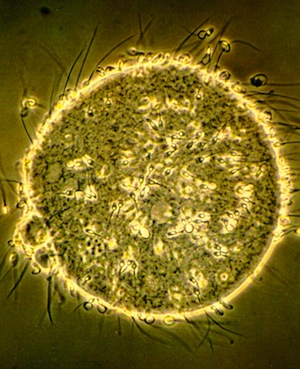
During a hamster egg penetration test, a lab analyst will evaluate your sperm samples using techniques that are similar to the techniques used in IVF. The only difference is that a doctor uses eggs from a hamster. A lab analyst will chemically treat hamster eggs to see if human sperm can penetrate them.
The prepared sperm are incubated with 15 to 20 chemically treated eggs. If your sperm is working how it should, it will be able to penetrating the eggs. The lab analyst will then count how many eggs were penetrated and calculate a percentage.
If fewer than 50 percent of the hamster eggs are penetrated, this means your sperm can’t fertilize eggs as well as normal sperm can. If more than 50 percent of the hamster eggs are penetrated, your sperm should also be able to penetrate human eggs.
Hormone Evaluation
If no sperm are found in your semen or if the count is extremely low, we may use a blood sample to evaluate hormone levels (FSH, LH, free testosterone, and total testosterone and prolactin). Clues from these tests may lead to possible causes and the best therapies.
Kruger or “Strict Criteria” Morphology
Hypoosomatic Solution Assay
The hypoosomatic solution assay tests a sperm’s how well your sperm functions and whether your sperm is viable (can penetrate an egg). This test specifically examines the sperm’s plasma membrane and how well it works, which may reveal its fertility.
First we will examine your seminal fluid’s consistency and your sperm’s motility (movement). It’s normal for the seminal fluid to have a small number of white blood cells, but a larger number of these cells may be an infection or prostatitis (inflammation of the prostate). If your white blood cell count is higher, we may take a semen culture to diagnose and treat the problem.
Post-Coital Test
Five to 10 percent of fertility problems among couples are caused by irregularities in the cervix and its secretions. In order for sperm to successfully move through the cervix, the sperm must be able to penetrate the mucus surrounding the cervix. The lower cervix helps store sperm and releases it into the upper tract of the cervix before it enters the uterus.
The physical and chemical properties of cervical mucus change depending on where a woman is in her menstrual cycle. These changes affect the pH, viscosity, volume, cell content, and spinnbarkheit (measurement of stretch ability) in the cervical mucus. These changes can make the cervix more or less receptive to sperm penetration just before ovulation.
Retrograde Semen Analysis
We may recommend a retrograde semen analysis for men with a low sperm count. (An initial semen analysis will show if you have a low sperm count). Retrograde ejaculation is when sperm ends up in your bladder. If you have retrograde ejaculation, sperm will be in your urine after you have sex.
Many men with retrograde ejaculation have had an earlier surgery or medical condition that makes them more likely to develop retrograde ejaculation. Many things can make you more likely to develop retrograde ejaculation. These may include the following:
- testicular cancer surgery (RPLND)
- transurethral surgery of the prostate
- childhood bladder surgery
- diabetes
- MS
- spinal cord injury
Semen Analysis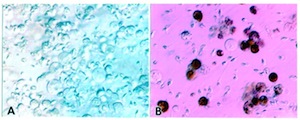
- sperm concentration (how many sperm are in each milliliter of semen),
- a motile sperm count (how well your sperm move and swim),
- and study of sperm morphology (shape).
Your sperm count is a measurement of how much sperm moves towards the egg—in other words, how much sperm is available to fertilize an egg. Lower sperm concentration, along with how well your sperm move and swim (also called sperm motility), can also affect your motile sperm count. The shape of your sperm (morphology) is also important since sperm that are shaped incorrectly have a have a harder time fertilizing eggs.
A normal semen sample is usually made of 35 percent normal, correctly shaped sperm. The other 65 percent of sperm are often abnormally shaped or abnormal. A smaller percentage of normal sperm could cause infertility problems.
Learn more about semen analysis testing.
Semen Culture
A semen culture may be created If you have an increased number of white blood cells in your semen sample, your doctor may ask you to get a semen culture. To make a semen culture, a lab analyst will culture your semen sample for bacterial growth. If bacteria are growing in your semen sample, your sample will be sent to another lab to identify the type of bacteria and what antibiotics can kill the bacteria.
If you’d like more information about the presence of white blood cells in your semen, contact us.
Sperm Aneuploidy by FISH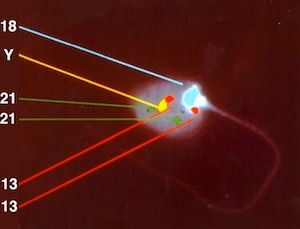
Sperm Chromatin Integrity Test (SCIT)
SCIT tests analyze the quality of your chromatin and whether there are any breaks in your DNA strands. Chromatin is a bundle of genetic material inside your cells and includes DNA, RNA, and prortein. Both of these things have been shown to affect an embryo’s quality.
Lab analysists usually find DNA breaks during chromatin remodeling. But if your DNA strands are broken, this damage will be repaired during the late stages of spermatogenesis. If the damage is not repaired, DNA breaks inside your sperm may affect your sperm’s ability to fertilize an egg. DNA breaks can also affect the quality of embryos.
The SCIT sample is divided into two portions. One portion will be used to evaluate DNA damage. The second portion will be test density gradient centrifugation. In the final part of the test, our lab analysists will see if DNA in your sperm are damaged.
Sperm Longevity
How long your sperm stay functional after ejaculation could cause fertility problems. The sperm longevity test can check how your sperm are working after they’ve been washed free from the seminal plasma and stored in a solution.
Transmission Electron Microscopy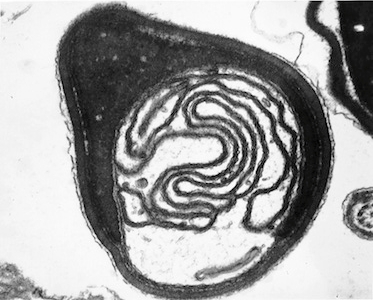
Varicoceles
Varicoceles are swollen veins in the scrotum. They are found in fertile as well as infertile men and are extremely common. But since they happen more in infertile men, they could harm fertility. Varicoceles are often found when there are fewer normal sperm and more tapered or abnormal sperm.
It also seems to be associated with lower sperm concentration and motility. Like other forms of infertility, varicoceles don’t cause complete sterility. But they can cause reduced fertility, which means it will be harder for you and your partner to get pregnant.
You may be referred to a urologist If the results of your semen analysis look like the semen found in men who have varicoceles. The urologist will evaluate if you have a varicocele (usually directly above the testicle) and determine the best treatment. You may not need treatment.
If the varicocele is affecting your plans to have more children, your doctor may suggest fertility treatment options. A surgical procedure called a varicocelectomy may be performed (on an outpatient basis) to correct the problem.
If no sperm are found in your seminal fluid, we will run a test to see if any fructose is in your seminal fluid. If you don’t have any fructose, there may be a blockage in the vas deferens, which secretes fructose and carries the sperm from your epididymis to your prostate gland.
