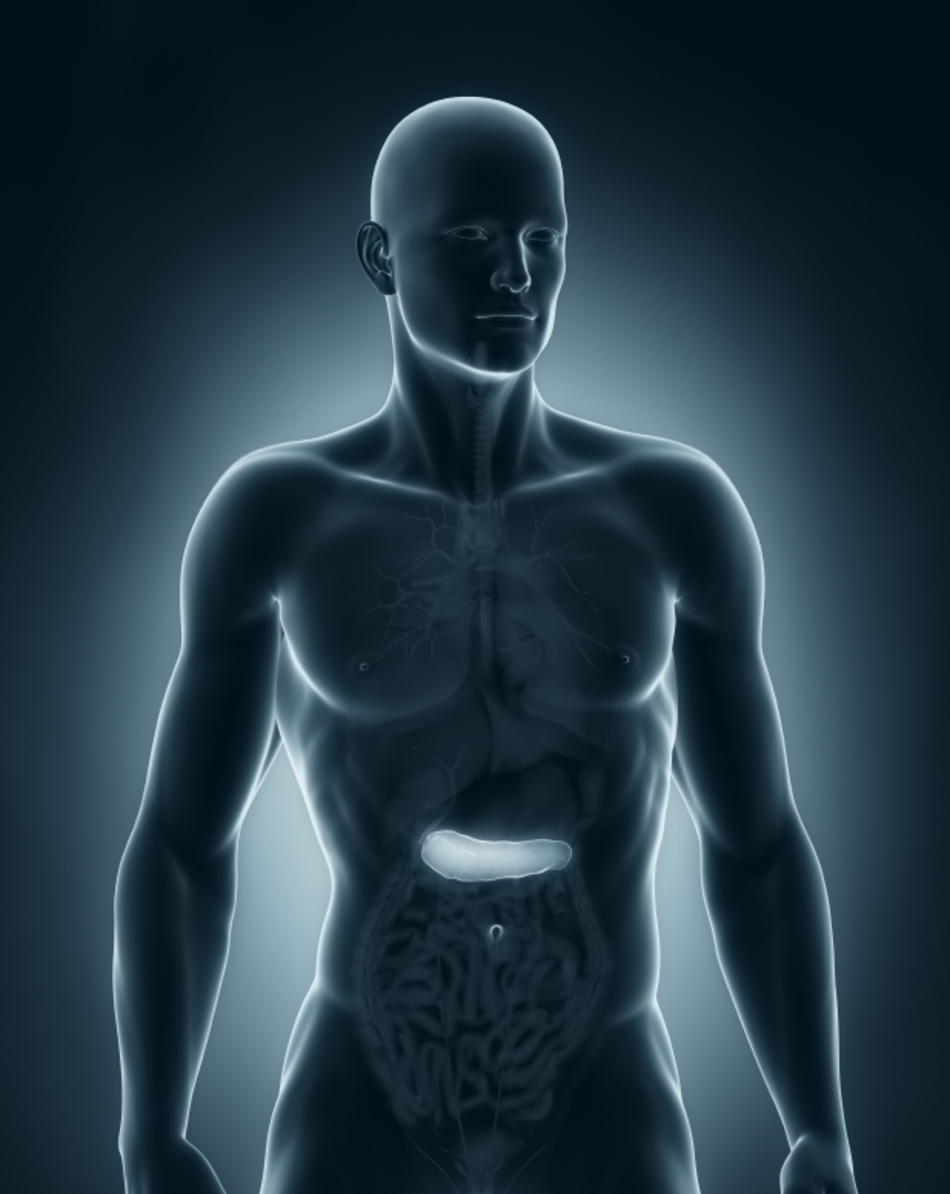
Dr. Miller: Pancreatic neuroendocrine tumors and hepatic transplants. We're going to talk about that next on Scope Radio.
Announcer: Medical news and research from University of Utah physicians and specialists you can use for a happier and healthier life. You're listening to The Scope.
Dr. Miller: Hi, I'm Dr. Tom Miller and I'm here for Scope Radio with Dr. Thomas Chaly from the Department of Surgery. Thomas is a transplant surgeon and he also specializes in metastatic neuroendocrine pancreatic cancers.
These are rare cancers, Tom, as we've talked about in a previous session and my understanding is that in certain cases one might transplant the liver in order to cure a metastatic neuroendocrine tumor of the pancreas.
Dr. Chaly: That's correct. So in instances where resection or interventional radiologic methods are not applicable to certain patients, University of Utah has shown excellent results in transplanting, in whole liver transplantation of these patients, and with a great long-term survival.
Dr. Miller: Would you initially debulk the tumor in the liver, or would you decide to go straight to hepatic transplant?
Dr. Chaly: That's an excellent question. Debulking is one of the primary modalities, and if we could debulk the tumor safely, leaving enough liver remnant, we would do that. But in instances where debulking wouldn't provide a benefit to the patient, transplantation is the next best option.
Dr. Miller: Do you debulk first and then in some cases transplant later, or is that generally not done?
Dr. Chaly: No, that is done. Debulking can offer a temporary solution of patient symptoms, and if this is not successful and there's a recurrence in the immediate post-operative period, approximately six months, we may consider transplantation at that point.
Dr. Miller: Now perhaps for the audience we should distinguish this from regular or more common pancreatic cancer. You would not debulk or transplant a patient with what we know as common pancreatic cancer.
Dr. Chaly: That is correct. Pancreatic cancer, or pancreatic adenocarcinoma, is extremely aggressive and debulking or transplantation, given the immunosuppression that the patient's on, would be of no benefit.
Dr. Miller: So these neuroendocrine tumors, some are functional, that is, that they produce hormones and cause symptoms, and others are silent. I think you like to use the term ninja cancers. I think you might say that the ones that are less functional or not functional, that is, they don't produce hormones, are the ones that actually metastasize more frequently?
Dr. Chaly: Well, that's correct that they metastasize a little more frequently, and that happens primarily because they're so silent and they're not producing hormones, so we're unaware of their activity. And so at this point, after the primary tumor has been controlled, a liver transplant is an option in some of these patients.
Dr. Miller: What percent of patients with neuroendocrine disease in the liver, metastatic disease in the liver, would undergo a transplant versus the debulking that you talked about previously?
Dr. Chaly: I would say the vast majority of patients would actually undergo a surgical debulking, and in select patients where debulking wasn't an option, maybe less than 10% transplantation would be available for them.
Dr. Miller: But if that's the case, it sounds like the University of Utah would be a great place to have that treatment.
Dr. Chaly: Absolutely. We've had an excellent experience in transplanting these patients and have had a great success rate, and these patients have done well over the long-term period.
Announcer: TheScopeRadio.com is University of Utah Health Sciences Radio. If you like what you heard, be sure to get our latest content by following us on Facebook. Just click on the Facebook icon at TheScopeRadio.com.


