Dr. Miller: You've had a hip or knee replacement and need a revision, we're going to talk about that next on Scope Radio.
Announcer: Access to our experts with in-depth information about the biggest health issues facing you today. "The Specialists," with Dr. Tom Miller, is on The Scope.
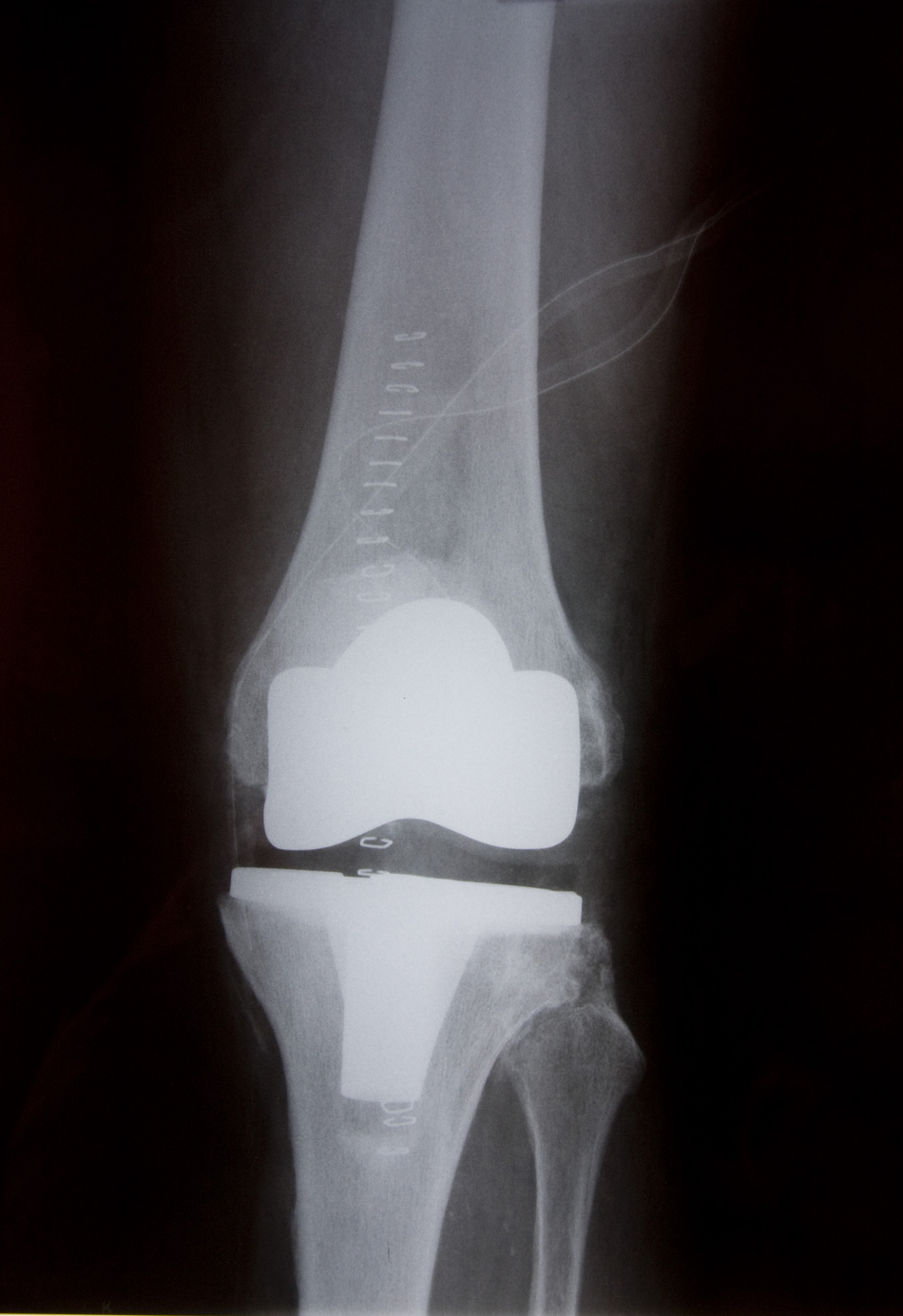
New Technology for More Durable Joint Replacements
Dr. Miller: Hi, I'm here today with Dr. Chris Pelt. He's an orthopedic surgeon here at the University of Utah in the Department of Orthopedics. Chris, talk a little bit about how long a hip or knee replacement lasts. Obviously, that's pretty variable. But when that begins to wear out, and I'm sure in a certain percent of people it does, what's the next step?
Dr. Pelt: Historically, a hip replacement would last 10-15 years. Newer technologies have been developed, which allows the hip replacements to be lasting closer to the 30-year time point, when we look at these on wear simulators, we haven't had the technology 30 years now, but when we look at the available information and literature it looks like it could last much longer than historically.
Common Sources of Wear on Replaced Joints
Dr. Miller: So when they wear out, does the actual prosthetic device wear out or do they come loose? What actually happens? What's more common?
Dr. Pelt: There are three main wear mechanisms or failure mechanisms. One is that the bearing will wear out so the plastic liners can get worn and you can replace the plastic liners. More commonly, however, what we find is that the implants can get loose from the bones or the worst of all of the complications would be infections of the implants. And a lot of the referrals that we do see come from outside in the community hospitals, they refer to us for complications related to infections.
It's one of the more common failures in early time points when a joint replacement fails, but it can happen later in life as well, it can happen when bacteria get into our bloodstream and they find their way to the artificial joints. Metal and plastic do not have an immune system so when bacteria are in our bloodstream, whether it's from an infection in our mouth, dental work, an infection of a toe or any other type of infection in our body, a bacterial infection, it can find its way to our hip replacements. We want to be careful about that when patients are undergoing treatments for other medical issues.
Revising Previous Joint Replacements
Dr. Miller: Well, based on how patients present with either one of those three things, I guess you craft the repair or surgery to meet that problem. I would imagine a revision surgery is probably a delicate or complex surgery compared to an initial hip replacement or knee replacement.
Dr. Pelt: It's quite a bit more complex. It takes a little bit more expertise and skill because it can be very easy to have a revision surgery and have things go wrong.
Dr. Miller: How long, then, does that revise tip last? Does it last as long as the initial implant or are people looking at a little less lifespan on the hip or knee?
Dr. Pelt: It depends. It depends on what the problem is that we're treating and what implants we have to use to deal with that reconstruction. But, on average, they should last similar time frames to the initial index operation. Some of these will be, hopefully, the last surgery the patient needs to have in their lifetime.
Preventing Joint Replacement Infections
Dr. Miller: Now, patients who present with the infected hips, I think you probably take the old device out and then either put in a new device or wait until the infection has been treated. But I imagine that treatment goes on for several weeks with antibiotics. Is that right?
Dr. Pelt: That's right, yeah. We've taken a lot of pride and created a significant team around the treatment of joint replacement infections here at the University of Utah. We have infection disease specialists, our internal medicine colleagues, ourselves as orthopedic surgeons, our nurses, physical therapists, physician assistants and a bunch of other people that help us take care of our patients. But yeah, the surgery is required initially to take the device out and get rid of all the bacteria out of the joint.
We place a temporary antibiotic-laden or antibiotic-containing spacer with some temporary parts that'll allow the hip or knee to still move the way it typically would and after about three months of treatment with antibiotic and a drug holiday, we often will be able to take the temporary device out and replace it with a permanent device again.
Recovering from Surgery
The typical revision joint replacement surgery we may not allow to bear weight on the limb that was just operated on right away. Often, after a primary hip or knee replacement, we have the patients up and walking, with full weight bearing, the day of the surgery. With revision surgery, depending on what it is we are doing, but with most revision surgery, that often is delayed. So we won't let them . . .
Dr. Miller: Both knees and hips?
Dr. Pelt: Both knees and hips. Typically for about six weeks. And the reason is as we mentioned when we are dealing with bone loss and having to accommodate or account for that with bigger and larger implants, sometimes, we need biology to be on our side.
Dr. Miller: It's almost like a fracture that needs treatment so you can put weight on it.
Dr. Pelt: It's almost like treating a fracture. Exactly. So we're waiting for bone in-growth to happen to the implants before we start putting too much weight and start making micro-motion or something that could compromise the stability or fixation. So typically, they're going to be at least six weeks behind where they might have been after their index or primary joint replacement surgery.
After which time, we start ramping up some more of their physical therapy, start getting walking on it, start getting them to strengthen their muscles with some weight and resistance modalities finally, where they probably have not been doing those in the first six weeks. And so they can just expect a little bit long time point until they get back to their maximum improvement point.
Dr. Miller: Initial replacements, they are out of the hospital pretty quickly these days. How long would they expect, on average, to be in the hospital after a revision?
Dr. Pelt: Our typical primary joint replacements will go home the next day, sometimes the latest two days after surgery. A revision surgery has an average length of stay of around three days. Some patients will go home around day two, others around day three, sometimes even day four, but about a day or two longer in the hospital. That's mostly because they're trying to account for the weight bearing restrictions, the mobility needs that they have to get used to after having the revision surgery. So our physical therapists are going to be working with them in the hospital, trying to get them to do the things that they'll need to be able to do when they get out of the hospital
Getting Proper Physical Therapy Post-Op
Dr. Miller: Now, you have patients coming from cities distant to Salt Lake. So, interestingly, once they leave the hospital, how do you make sure that the therapy they are getting in their hometown is going to be adequate?
Dr. Pelt: So we have patients that fly in from northern Montana, Wyoming, Idaho, Nevada, Colorado, Arizona, New Mexico all to have their surgeries done here with us. And it is difficult. We do have, like I said earlier, we do have a big team, including some of our care coordinators and our nurse coordinators that help kind of reach out and make sure our patients are doing well after surgery. We call our patients pretty frequently.
We write pretty strict and standardized protocols and instructions to send home with our patients when they leave the hospital so the physical therapists are able to follow those directions pretty closely. And that way, we don't compromise anything that may be a difference in how they treat things in one place vs how we do here. We try to give them those instructions so it is very clear on what our expectations are when they leave the hospital. And then our team of care coordinators and nurses are going to be calling and ensuring that everything is going right as the weeks progress.
Dr. Miller: So their therapist, no matter where they would be, would be able to contact your care team to figure out if there we any things that they need to modify or revise in terms of the treatment?
Dr. Pelt: Absolutely.
Announcer: Thescoperadio.com is The University of Utah Health Sciences Radio. If you like what you heard, be sure to get our latest content by following us on Facebook. Just click on the Facebook icon at thescoperadio.com
Orthopedic Services Near You
Receive the same great care from the same specialists at both locations.
University Orthopaedic Center
Located in Salt Lake City, Research Park
South Jordan Health Center Orthopedics
Located in South Jordan, Daybreak



