This content was originally produced for audio. Certain elements such as tone, sound effects, and music, may not fully capture the intended experience in textual representation. Therefore, the following transcription has been modified for clarity. We recognize not everyone can access the audio podcast. However, for those who can, we encourage subscribing and listening to the original content for a more engaging and immersive experience.
All thoughts and opinions expressed by hosts and guests are their own and do not necessarily reflect the views held by the institutions with which they are affiliated.
Interviewer: Your child was diagnosed with pectus excavatum, which is also referred to as funnel chest. It's a caving of the chest. And you want a second opinion about whether your child should have surgery or not.
Dr. Stephen Fenton is going to help us better understand when surgery might be the best option.
Is Funnel Chest a Cosmetic Issue?
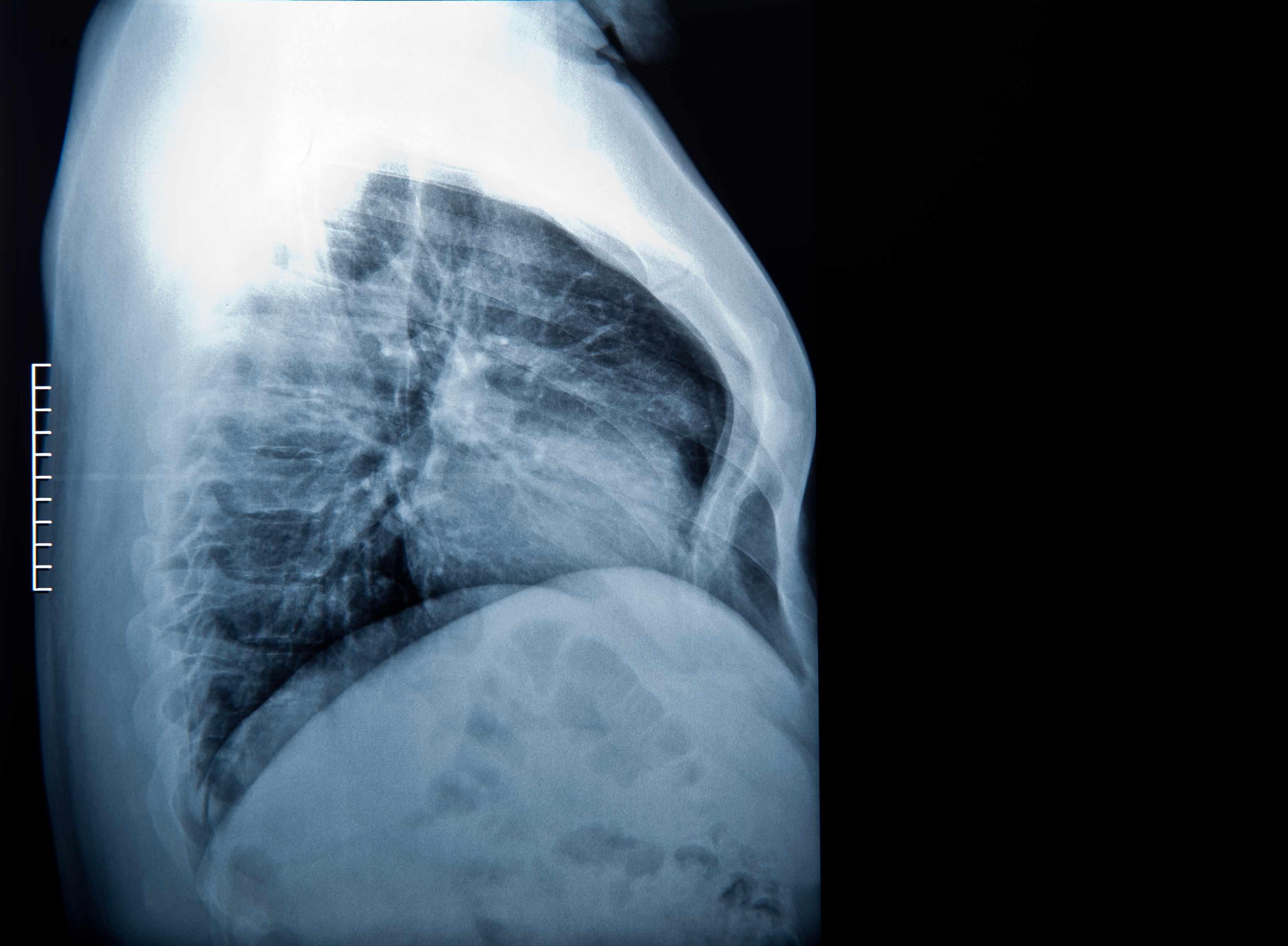
So when the chest area is caved in, the condition is called pectus excavatum. Does that offer any other sort of health threats, or is it purely just a cosmetic issue?
Dr. Fenton: No, it actually does. So it's part of the congenital pectus deformities, which encompasses funnel chest as you talked about it, pectus excavatum. I oftentimes refer to parents or kids as think of a backhoe that's excavating. It's digging, and so the chest goes inward. The other disorder is pecutus carinatum, which is where the chest comes outward.
Health Conditions Associated with Funnel Chest
Excavatum is associated with other conditions. And so, whenever I see a child in consultation, I always try and ascertain whether any of those conditions are present. So, for example, scoliosis is associated with it. Mitral valve prolapse, which can oftentimes be brought on, or recognized by a heart murmur, is also associated with pectus excavatum. Also, Wolff-Parkinson-White is an abnormal pathway in the atrium of the heart, which can cause heart arrhythmia.
So some of the questions I always ask are, "Is there a history of murmurs in the child, or any of the parents? Is there a history of scoliosis? And has he or she ever felt their heart race just out of the blue, not with exercise?"
So the last thing is a connective tissue disorder, Marfan syndrome. These individuals who have this often have laxity in their joints. Sometimes they can lens dislocation of their eyes. They often have dilation of their aorta, as well as some cardiac valve problems. They're oftentimes very, very tall and have some features that we would refer to as Marfanoid. In that case, if we're ever worried, and I do ask parents specifically if there's a history of Marfan syndrome in their family, we would refer them to a geneticist to make sure whether that's present or not.
Interviewer: The heart conditions you talk about, and some of those other conditions, is that because the chest is caving in and putting pressure on that cavity? Is that what's happening?
Dr. Fenton: So we do know that there is pressure on the chest, and oftentimes a murmur can happen because of the heart being displaced and/or pushed on. But these entities are associated with pectus excavatum and not really caused by them.
Interviewer: So fixing that condition does not necessarily fix the other conditions?
Dr. Fenton: Correct. And so, in those conditions, if we feel like there might be mitral valve prolapse, we would get an echocardiogram, or an ultrasound of the heart, to look for that valve disease, because that's something that a cardiac surgeon would have to fix, or follow and maybe subsequently fix, but not something that would be corrected by correcting the pectus itself.
How Early Does Funnel Chest Appear in Children?
Interviewer: When might a parent notice that this is a condition that their child might have?
Dr. Fenton: Pectus excavatum is actually noticed oftentimes when kids are young. In fact, most parents come in and they'll say, "Oh, yeah, we saw it when he was a baby. It was like a little divot or dip in the chest." But for most kids, it really starts to become prominent and more noticeable once they start their growth spurts around or after puberty. And that's what causes it. It's actually growth from the costal cartilage where it attaches to the sternum, and there is a differential in growth, which causes the sternum to go inward.
When is Surgery Needed to Treat Funnel Chest?
Interviewer: So let's talk about now what you would do for somebody that has pectus excavatum, the sunken-in chest. It's usually taken care of by surgery, if I understand. How do you know if surgery is something that you would do for a particular patient?
Dr. Fenton: So, first of all, there is a range. Sometimes it can be very mild. It does go inward, but the child doesn't have any symptoms. They don't complain of chest pain, shortness of breath, or back pain, all of which can be associated with it. They feel like they can keep up with their classmates or their teammates when they play sports. And in that case, I usually say, "Don't do anything."
In boys, especially, I'll tell them, "Hey, work your upper body, build up your pec muscles, and a mild pectus will actually make you look more ripped." You'll look like . . . you won't necessarily have to do anything, especially if it's not limiting to their activities, and especially if they are totally symptom-free.
Now, on the other end, with severe pectus, it's interesting. I've seen kids who, let's say, have played competitive sports, basketball, football, soccer, track, etc., and even when they notice it before they hit puberty, or right when they're hitting puberty, they'll often tell me adamantly they can keep up with their classmates or their teammates.
And then as we follow them, and the pectus becomes more severe, even they and their parents will definitely start saying, "You know what? They're putting in as much effort as they were before, but they fatigue early, they complain of chest pain, they complain of shortness of breath, and they tire out much quicker than their teammates do."
And a lot of that can be attributed to the severity of the pectus. It does displace the heart. It can displace lungs, etc., and there is this sense of not being able to catch your breath or breathe appropriately. In that case, with severe pectus and with symptoms, I would typically recommend surgical repair.
Ideal Age for Funnel Chest Surgery
Interviewer: Is there an optimal age to do the treatment, or is it more just watching the progression of the condition?
Dr. Fenton: We usually say around 13 to 15 years of age. That does not preclude kids that are either younger or older. But around that age, the chest is just very malleable and they usually tolerate it a lot better.
Interviewer: So it sounds like, with symptoms, you would definitely consider the surgery. Without symptoms, if everybody is feeling okay about it, then perhaps surgery would not necessarily be an option.
Dr. Fenton: Correct. And I think the important part of that is for the young adult and the parents to seek consultation. Along with the surgeon, we can talk about what the options are, whether we want to continue to follow, whether we would recommend repair, or whether nothing needs to be done at all.
Funnel Chest Surgery Procedure
Interviewer: And the surgery, is it a pretty complicated surgery? I mean, is it a major surgery?
Dr. Fenton: Dr. Nuss and colleagues came up with a procedure that we would term "minimally invasive." So a small incision on either side of the chest, about an inch and a half to two inches, and then using a camera we can actually skirt the bar underneath the sternum. And then when we turn the bar around, it brings the sternum out. And we secure the bar in place.
Even though it's minimally invasive, and that's nice because whenever it's minimally invasive the body can recover quicker, the sternum does not want to be pushed out. And so there is pain associated with it. We work closely with our anesthesiologist to help make sure that we can mitigate that pain as much as possible.
And we've really done a much better job in the last several years. Kids who are undergoing this are leaving the hospital quicker and are recovering faster. This approach is, again, a great approach. It has a very low infection rate. It has a very low complication rate, and the outcomes in the long term are very good.
Recovering from Funnel Chest Surgery
Interviewer: Does that pain continue during the treatment, then, after the procedure?
Dr. Fenton: No, usually the worst of it is for the first few days. So they're oftentimes in the hospital, and, again, our anesthesiologists help us control that pain. Most kids I say, by the time they come see me about two weeks afterward, are for the most part back to normal. As with any major surgery, I always say, "There might be a little bit of pain or a pull for about six to eight weeks afterward." But once you've made it past, really, a month or a month and a half, those young adults are back to normal.
Interviewer: So this sounds like a very specialized individual that would do this. If somebody is more in a rural area and they want to have this procedure done, they're going to have to go to a metropolitan area it sounds like?
Dr. Fenton: Absolutely. I mean, the procedure itself is important being able to know how to do it, how to manage outcomes, etc. It's also very important to know when to offer the operation and when not to as well, and the further workup around it.
And so, when seeking a surgeon, you want a surgeon who does this often, who cares for these kids often, and also works in a system that does, because it's much more than just the surgeon. It's the OR team. It's the anesthesiologist. It's the nursing staff, etc., that all contribute to good outcomes for these kids.
Interviewer: Final thought for somebody who is listening to this, who they believe that their child might have this condition?
Dr. Fenton: Final thought is, first, it's not dangerous. Don't restrict the activity of your child. And two, we're always happy to take a look at it and determine whether it's something that's not going to cause any problem for them or that might require surgery, and certainly can provide the expertise to do so.
updated: September 10, 2024
originally published: February 9, 2021