Episode Transcript
Interviewer: In 2021, the guidelines for lung cancer screening changed to be even more effective at prevention. And to better understand lung cancer screening and how these changes impact you, we're joined by the Associate Chief Medical Quality Officer at Huntsman Cancer Institute, Dr. Thomas Varghese.
Dr. Varghese, I understand the new guidelines have three specific steps to determine if a person should be screened for lung cancer. Let's start with those three things.
Three Steps for Determining Eligibility for Lung Cancer Screening
Dr. Varghese: The three different steps include, one, adults between the ages of 50 to 80 years of age; two, who have had a 20-pack-year smoking history; and three, who are currently smoking or have quit within the last 15 years.
Interviewer: All right. And on that guideline, what is pack-year history? What does that mean?
Understanding Pack-Year Smoking History
Dr. Varghese: A pack-year history means those who have smoked a pack per day over the course of a year.
Interviewer: And if I've smoked two packs per day, would that mean it would only have to be 10 years that I smoked . . .
Dr. Varghese: That is correct.
Interviewer: . . . to have a 20 . . .
Dr. Varghese: A 20-pack-year history. Yeah, that is correct.
Interviewer: So three packs a day would be . . . Okay.
Dr. Varghese: An even shorter period of time.
Changes in Lung Cancer Screening Guidelines
Interviewer: Got it. So what in the guidelines changed just recently?
Dr. Varghese: There were two things that changed in the guidelines. First, the age cutoff dropped from age 55 down to age 50. And the second is the smoking history was reduced from a 30-pack-year to at least a 20-pack-year.
Interviewer: All right. And why did that change?
Dr. Varghese: Part of it was that we realized that we were missing out on a high-risk population. And as a result of it, once guidelines are assessed . . . They're not permanent tablets in stone. They continuously undergo monitoring, revision, and adjustment as needed. And as a result, these were the two changes that were made.
The Relationship Between Smoking and High Risk of Lung Cancer
Interviewer: What I'm seeing here is it looks like perhaps it was revealed that you don't have to smoke as previously thought to be at a high risk of lung cancer.
Dr. Varghese: That is correct. And I anticipate that there may be even further changes in the years ahead. We have ongoing research always trying to identify high-risk patient populations. And so we know that currently these are where the guidelines sit, but they're going to be constantly monitoring and potentially revising that in the years ahead.
Interviewer: And if a person's listening, do they have to have all three of those things apply? They need to be 50 to 80 years old, 20 or higher pack-year history, and currently, smokers who have quit within the past 15 years.
Dr. Varghese: Currently, yes, if they truly have no other medical history. Now, this is where sometimes the guidelines get a little bit fuzzy and that's why you need to work with your physicians to see where you would potentially qualify.
So for example, let's say you have a very strong family history of lung cancer. Those are patients that we're not waiting for age 50. Let's say that in your family you see that there was lung cancer that was occurring at the age of 40, for example. Your physician may decide to start that screening process well ahead of what the guidelines currently are out in the press.
Insurance Options for Lung Cancer Screening
Interviewer: And if I understand correctly, if you're within those guidelines, most private insurance would cover that screening.
Dr. Varghese: That is correct. And that's one of the biggest things. When it's guideline-concordant care, insurance companies have no problems covering those issues. But this is, again, where working with your physicians can really help because if your physicians identify that you have risk factors outside of these guidelines, they can work with insurance companies to get approved cancer screenings.
Interviewer: And how is this screening done?
The Process of Lung Cancer Screening
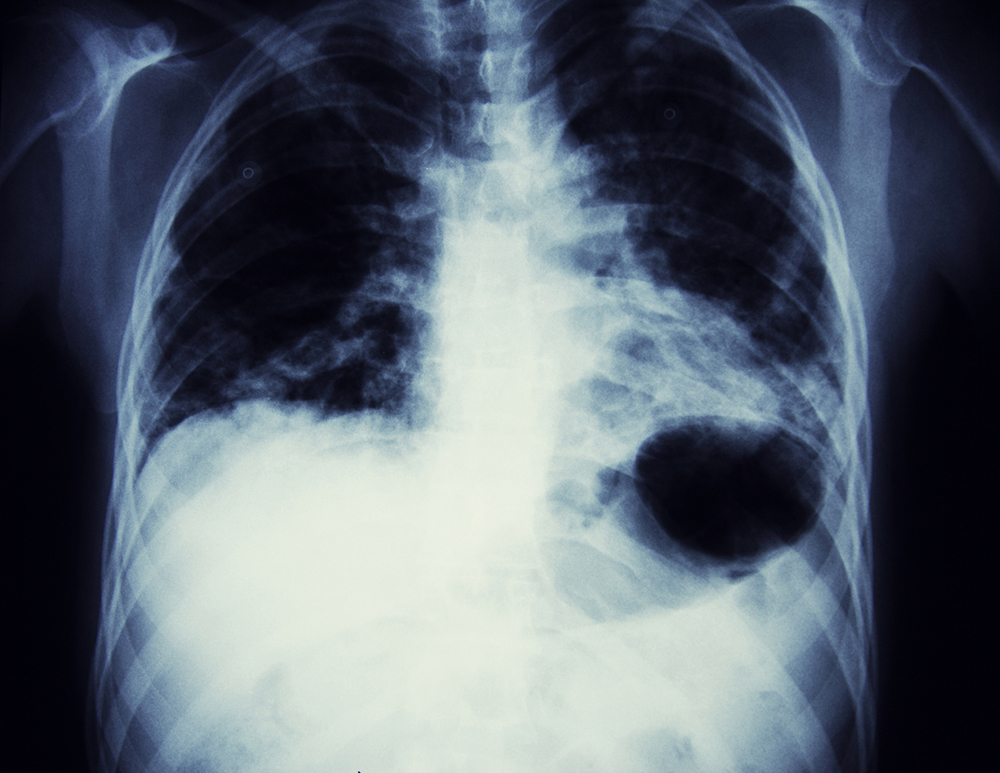
Dr. Varghese: The screening is done by the use of what we call a low-dose CT scan, computed tomography scan. And what it is, is that . . . One of the common questions we get is, "How quickly is the scan done?" It's very efficient. Most scans are done within minutes.
The second thing is that low doses are related to the amount of radiation that is being done. The technology has advanced so much that the amount of radiation per scan is really minimal amounts. And so there's only a minimal amount of risk for a patient to undergo a scan, to obtain the imaging.
Interviewer: And how accurate are the screenings then?
Dr. Varghese: They're incredibly accurate. And in fact, one of the amazing things is people as old as I who've been doing this for a while and everything, see that the technology keeps advancing and the sensitivity and the specificity of these scans continue to improve. And so they're quite accurate.
But in cases of doubt, what it really sets it up for is that if there's any suspicion, you can always end up following up with a follow-up scan at a short interval as well.
Interviewer: One of the concerning things about screenings that I think I didn't realize until more recently is it sounds like screenings are great, right? "I'll get the screening and there are really no downsides." This is not to discourage anybody from getting a screening, but there are potential downsides to the screening.
The test sounds like it's low-dose radiation, so that's not as big of a deal. But what about false positives? That's where people might end up getting procedures they don't need. Talk to me about that.
Dr. Varghese: Correct. I mean, this is where sometimes the technology becomes too sensitive. And so what it is, is that it shows an abnormality in the imaging, but what it really warrants is a conversation with an expert in the field.
And I think that this is where instead of getting worked up about an abnormal finding, really the most important part of this whole process is having that informed discussion, the shared decision-making about what to do next.
And so what we encourage everybody to do is not to have the imaging in isolation. Really, the key thing is to have the imaging, get the results, and have that conversation with your physician.
Interviewer: In the research studies, a lot of care is taken to make sure that the cancers that are found are actually dangerous. In the real world, that might not necessarily be the case. So how can you be sure that you have a professional who's going to help you navigate those false positives?
Dr. Varghese: Great question. I think that this is where the experience of the physician and the experience of the healthcare team really come into play. You hear terms such as high-volume centers or centers of excellence. And really what those are, are terms signifying the experience an individual physician or an individual healthcare team has with a particular condition.
So what you want to have done is lung cancer screening or any type of cancer screening done with a team that is experienced in managing a lot of different patients. And so that includes differentiating between what is a true positive from a false positive, trying to have the experience to follow guidelines to figure out if you find an abnormal finding in a CAT scan, what do you do next?
And this is where having those conversations with the physician . . . If you are not happy with those physicians, then seek care with those health systems that can appropriately provide you with the guidance to navigate the path forward.
Discussions and Decision-Making after Abnormal Findings
Interviewer: If you get a lung cancer screening and the physician says, "Well, I'm kind of skeptical about this particular finding that I found this nodule," and they suggest a biopsy, should somebody just go right to that or should there be more conversations before that?
Dr. Varghese: There should probably be an initial conversation beforehand. And the conversation really goes on to, "What are the features on the CAT scan that were raising your concern that this could be a cancerous lesion or not?" That's Step 1.
And then Step 2 really comes to the decision about what to do next. Is it just a short interval repeat of the imaging to make sure that the finding is real, or do you proceed forward with a biopsy of that lesion?
And this, again, is where the experience of the team comes into place. What I mean by experience includes the experience of the physician having that conversation with the patient, the experience of the radiologist or radiology team who is reading that CAT scan, and then, of course, obviously the experience of whoever's going to perform the biopsy as well as analyzing the pathology of the biopsy itself.
Interviewer: And then after a biopsy, if it's discovered that it is actually cancerous, that's not necessarily always a reason for concern either, because it could be a slow-growing . . . You said earlier if the imaging is getting so good at finding things, this might have been something that was never going to be an issue anyway.
Dr. Varghese: That's a great question. What happens is the cancer itself has a wide spectrum, coming from slow-growing to very aggressive and fast-moving. And so really what we're talking about first is what we call diagnosis. Is there a cancer? Yes or no? Trying to figure out what type of cancer it is. Is it a slow-growing cancer, or a fast-growing cancer?
And then we proceed onto what we call staging. What we're trying to find with staging is if it is indeed a cancer, are you talking about localized cancer or is it cancer that's spread to other areas?
All of these aspects are important in the next steps, which are trying to figure out what the cancer is, trying to figure out where we are in terms of staging, and then the decision about what to do with the cancer.
Scheduling a Lung Cancer Screening
Interviewer: If somebody's listening to this right now and they're thinking, "I'd like to take advantage of this. I'd like to get a lung cancer screening because I meet the particular guidelines or I have a family history," what would the next step be? Where would that individual go?
Dr. Varghese: So the two recommendations are . . . One is if they have an established relationship with a primary care physician, to have a conversation with a primary care physician themselves. That could make it very easy to do within the confines of . . . They likely will have links to lung cancer screening modalities or connections throughout their health system.
Now, if that is not possible, then the other opportunities include searching for high-volume centers, such as Huntsman Cancer Institute, where we have very robust lung cancer screening programs. Those are programs where patients can find out information about lung cancer screening, or even just give us a phone call, and we'll be able to get you connected to the appropriate resources to facilitate the same.
Interviewer: So a referral from your primary care physician is not necessary?
Dr. Varghese: Not 100% necessary. It helps, but you can just pick up the phone and give us a call or search the website and send an inquiry through the internet.
There are very robust lung cancer screening programs that are out there. There are also a lot of resources available through non-profit organizations such as the American Cancer Society, and Longevity. There are a lot of resources available as well.
The key is if you are suspicious, act on it. If you have any doubts, reach out and connect. If you're not happy with the conversation you're having with your established links to the healthcare system, tons of resources out there where you can get advice and get the help that you need.
We're living in a remarkable time. There are a lot of resources out there. If there's any doubt that you have at any time, please reach out. We're here to help you.