Episode Transcript
Interviewer: A study gives new insights into how good bacteria work with our body to promote digestive health - up next on The Scope.
Announcer: Examining the latest research and telling you about the latest breakthroughs. "The Science and Research Show" is on The Scope.
Interviewer: A study published in Cell Host and Microbe is causing us to rethink what the immune system can do, and how it interacts with the good bacteria that live on our bodies. I'm talking with three authors on the study: senior author June Round, assistant professor of Pharmacology at the University of Utah, and co-first authors Jason Kubinak, and Charisse Peterson.
Dr. Round, what's the take home message from what you found in your study?
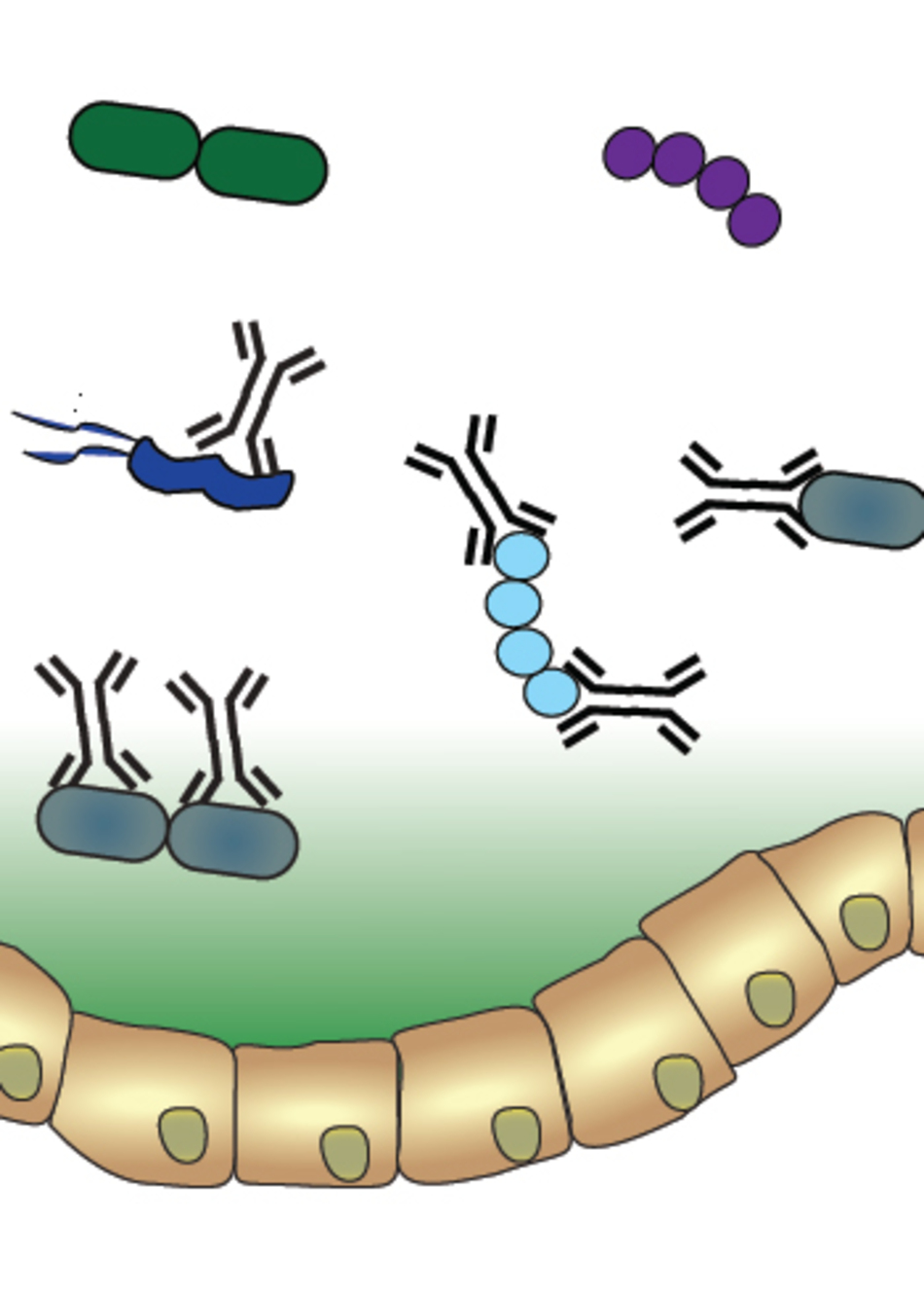
Dr. Round: I think the most important thing and the most interesting thing about this particular study is that it really highlights that there is a conversation between our immune system and the microbes that live on our body. It's becoming more and more clear that these microbes are very important for our health, and there's a lot of factors that shape what types of microbes can live on our bodies.
This study really highlights that our immune system has an effect on those types of microbes and that the microbes can send signals that tell our immune system how to develop, and in turn our immune system, as its developing, can also shape the types of microbes and the types of things that those microbes express.
Interviewer: Dr. Kubinak, how does that change our thinking from how we considered our microbiome before?
Dr. Kubinak: Well, I think within the last 10 years there's been a pretty significant shift in the way we view our interaction with the microbial world from initially primarily focused on antagonistic interactions where hosts and their immune systems were focused on eradicating and eliminating pathogens that make us sick. Whereas now, I think there's a renewed interest in the interaction between the hosts and microbes and how it promotes, or facilitates host health. I think our story sort of gets at that by demonstrating that the crosstalk between host and microbe generally is a health-promoting interaction.
Interviewer: So your work, in particular, addresses how the body keeps its balance of species of good bacteria intact, and you're particularly looking at one protein called MyD88. What did we know about this protein before your research?
Dr. Round: Its original function was assigned to recognize pathogenic organisms and basically act as the frontline detection to tell our immune system, "There is something going on here, there is a microbe here, so we better turn on our immune response and get rid of the pathogens." What we're really showing here is something very different, that detecting the microbe doesn't necessarily get rid of it here. It's actually helping to shape the types of organisms that live in the gut.
Interviewer: So how did you come to that conclusion?
Dr. Peterson: What did was we created a mouse that specifically knocked out this protein within a specific immune cell called a T cell. Then it gave us a unique opportunity to ask, what happens when this protein is absent in this immune cell and how does that affect the development of the microbiota as a whole in these animals.
Interviewer: So when MyD88 was knocked out of the immune system, it basically lead to an imbalance of the communities, the different species of bacteria in the gut. What does that do to the mouse, itself?
Dr. Round: What this lead to was that the animals themselves were more susceptible to inflammatory bowel disease, or an experimental model of inflammatory bowel disease.
Interviewer: I don't want to get too graphic, but what does that look like in a mouse?
Dr. Round: It's just inflammation within the guts of these animals. They lose weight.
Dr. Peterson: They get a severe wasting disease, and they get diarrhea.
Dr. Round: I think, for me, the most exciting part of the experiments was when we realized that this sensitivity to inflammatory bowel disease wasn't necessarily just caused by this defect that we had created in the host's immune system. One of the things that was driving this was actually this imbalance within the gut. Our ability to rescue that just by giving these mice healthy microbiota and rescue their disease susceptibility was, to me, the most exciting finding.
Interviewer: What do you mean? How did you fix the illness?
Dr. Peterson: So many people would refer to this as a fecal transplant. In the lab, we call this a microbiota transplant. You basically get rid of all those bad bugs that have developed in that animal because of their genetic deficiency and you replace them a healthy or with a balanced microbiota, so it's really a microbiota transplant. Obviously this is something that is starting to be done in people with various infections within their guts.
Interviewer: Well, right. I have to say, when I started talking about your work with other people in the office, that everyone became really excited when I said that I was going to be talking to you about fecal transplants, which sounds kind of strange. But, it's kind of this new exciting therapy that seems to have some pretty striking results in people as well.
Dr. Round: I'm glad to hear that people are excited about fecal transplants as, maybe disgusting as they sound. But to me, it makes sense. We have evolved for a very long time with these organisms, they promote our health, they're beneficial to us. So instead of using something that we chemically synthesized that's not natural, we're now using the microbiota as kind of a natural therapy to restore the balance in our bodies. So I think this is really a viable therapy in the future for multiple diseases, not just for inflammatory bowel disease.
Interviewer: I think one of the interesting parts of this study is that it really suggests that there is kind of a co-evolution between the microbiome and ourselves. How do you think about that?
Dr. Kubinak: To me, it speaks to the nature of natural selection to have driven the evolution of immune system machinery to promote benign symbiosis between us and our microbes.
Interviewer: So they're helping us, but we're also finding ways to help them.
Dr. Kubinak: Yeah, I think so. I think our immune systems have developed ways to definitely skew the community toward the presence of individuals who at the very least, are not going to cause us harm.
Announcer: Interesting. Informative. And all in the name of better health. This is The Scope Health Sciences Radio.