Episode Transcript
Dr. Jones: So you ran out of your birth control pills and the condom broke or something like that. You really don't want to get pregnant right now or anytime soon. What do we know about your options?
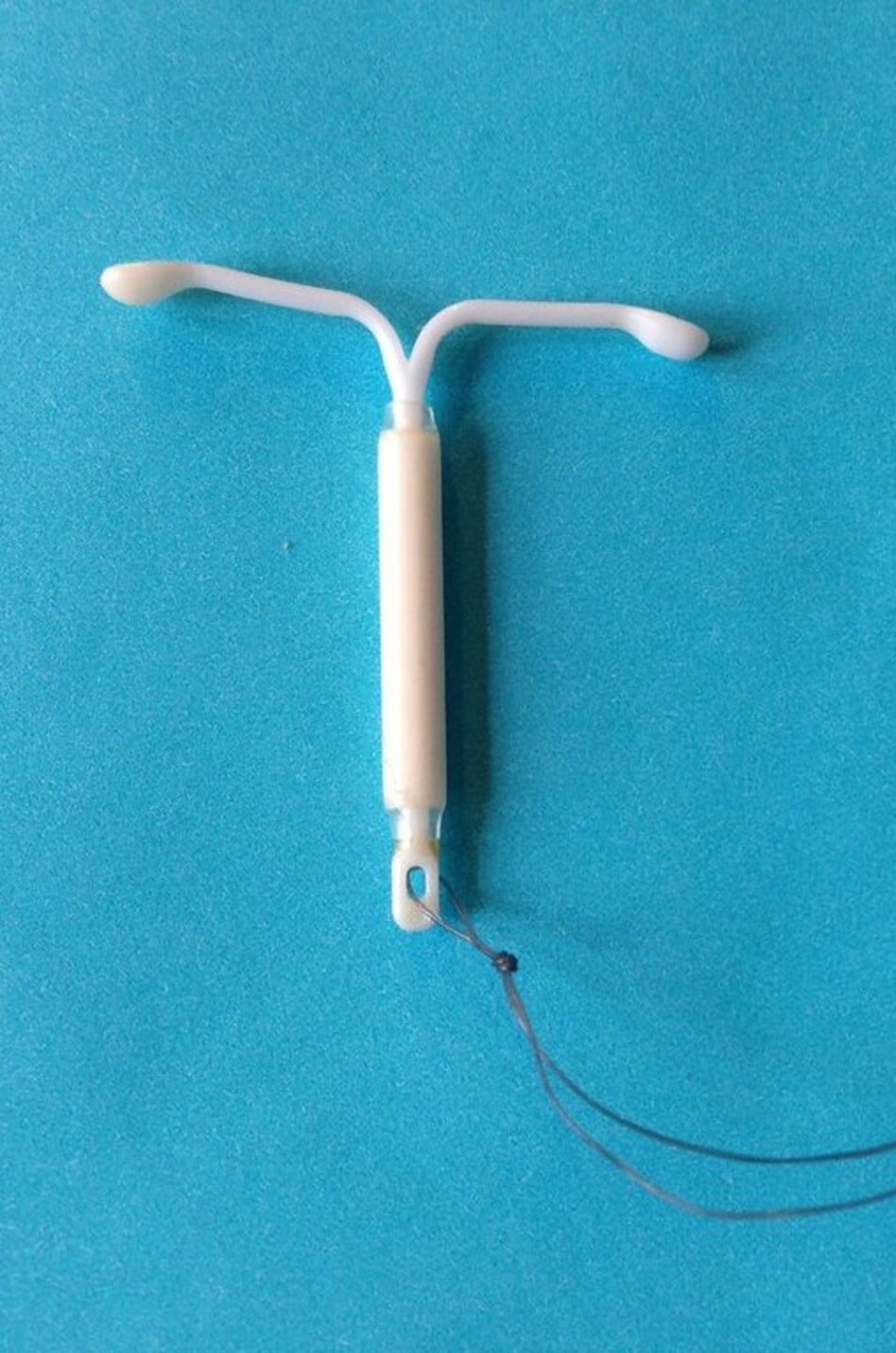
Many women know about emergency contraception, and many don't, something you can do to decrease your chance of pregnancy if you had unprotected or under-protected intercourse. There are two types of emergency contraceptions approved by the FDA that are available in the U.S., and they are pills, and they decrease the chance of pregnancy if they're taken within five days of unprotected intercourse. But there are other types of birth control that would work and keep on working if you're looking for contraception for more than this month.
With us today is Dr. David Turok. He is an OB/GYN specialist in family planning and chief of the division of family planning at the University of Utah. Thanks for taking some time for us, Dr. Turok.
Dr. Turok: Thank you.
Dr. Jones: What were the background reasons to ask the question of whether the levonorgestrel IUD, which is what we're going to be talking about, would work for emergency contraception? What made you do this question?
Dr. Turok: Well, I speak with people a lot about emergency contraception because I'm very interested in it, and I think it's amazing that you can use something after you've had sex to prevent pregnancy. And every time I talk about it with people during grand rounds or during educational presentations, people always, always, always ask . . . because we know we have great data to say that the copper IUD works very well for emergency contraception, people always ask, "Well, what about the hormonal IUD, the levonorgestrel IUD? Can you use that?" So 10 years ago, we started trying to gather data on this topic, and finally we have an answer.
Dr. Jones: So people came to the clinic wanting emergency contraception and they walked into the clinic thinking that they might get some pills. How did you get so many women to participate in the study when they came for just pills?
Dr. Turok: Like in many aspects of life, Utah is unique. And currently, one of the forms of emergency contraception pills is available without a prescription. You can just walk into pharmacy or supermarket and get them. Sometimes it's behind the counter, you might have to ask, but you can get it without a prescription.
In Utah, because there are many limitations for people, young people especially, with insurance coverage, people seek out the cheapest place to get it, and that is Planned Parenthood where there's a sliding scale and where people have known for a long time that they can get the pills.
And we've done a few different surveys and a few different kinds of projects where we offer people walking in for emergency contraception IUDs, and it's around 12ish percent of people are interested in an IUD in that setting. And that's, I think, potentially driven in Utah by the fact that people don't have adequate insurance coverage and they're looking for opportunities to get better methods of contraception. And when there are low or no-cost options presented, people are interested.
So, at the peak before Plan B, one of the pills was available over the counter. Planned Parenthood statewide distributed more than 50,000 doses of oral emergency contraception. So people know, and lots of people come to Planned Parenthood clinics in our state for the service, and when you present them with IUDs, some are interested in it.
Dr. Jones: So some of them are really looking for something for longer than just this month?
Dr. Turok: Exactly. Yes.
Dr. Jones: Right. So you've known that the copper IUD . . . we've all known from data that goes back 20 years, really, that the copper IUD works. So you then offered them either a copper IUD or a hormone-containing IUD. And what did you discover?
Dr. Turok: So what we found in this study where we randomized people to get one or the other type of IUD, either copper or the hormonal IUD, we found that the pregnancy rate was low, very low, in both groups in the month after.
So with copper IUDs, we had 321 people who were assigned to that, and we got one-month outcome data on. And we expected in that group, zero or one would have a pregnancy. And it was zero.
And with the levonorgestrel group, we really didn't know. We had built into the study stopping points. Like, if there were a bunch of pregnancies early on, we were just going to stop. But what happened was there were 317 people who got the levonorgestrel IUD and there was one pregnancy. Lower than we thought and much better than the pills.
Dr. Jones: Right. That's important because the methods that are currently FDA-approved, that those 50,000 women who came to our clinics seeking pills, the failure rate or the ineffectiveness rate is much higher than what you found with the IUDs, either one of them.
Dr. Turok: Yeah. To me, one of the very cool things about the study is the other studies that got FDA approval for those oral methods, these were things that took a long time and hundreds of millions of dollars were spent to go through the FDA process to get that approval. And in this study, we took a method that was already FDA-approved and we just showed that it works for this as well.
And the upside relative to the pills is, as you know, that people who are getting this can get . . . this is not just better than the pills for this one event, but you can continue to use it as long as you want, up to seven years, or for the copper IUD, up to 12 years. And that is a set-it-and-forget-it method.
Then for the LNG IUD, there's this side benefit, which is why it's more popular than, I think, the copper IUD, in that it dramatically reduces or eliminates both menstrual bleeding and cramping. And that is a big upside. And that's why I think people really wanted an answer to this.
Dr. Jones: Well, we have some evidence from another big study that just gave women what they wanted when they asked for contraception and then followed them, that the IUDs were something like 20 times more effective than birth control pills in preventing pregnancy?
Dr. Turok: Correct.
Dr. Jones: So if a woman comes to our clinic for an emergency contraception and she wants long-term reliable contraception, would she be offered an IUD, do you think, in our clinics? Because now that the work was done around here, I'm hoping that our clinicians know that it's an option. Do you think it's going to be used in the clinics?
Dr. Turok: I want to say absolutely.
Dr. Jones: I do, too.
Dr. Turok: But I would also say as our team is working on getting this paper published, I would occasionally have these pangs of terrible thoughts that 10 years down the road, it's going to be like the authors of this paper and 10 other people that we know that know about this and nobody is going to ever have done any of it.
And so I started making lots of phone calls and sending lots of emails to people who I thought would be critical partners in disseminating the information. And one of the things that helps get the word out a lot is getting the paper published in a high-impact journal.
Dr. Jones: Right. It was published in "The New England Journal of Medicine," which is probably our premier medical research journal, I think, in the United States, or one of them.
Dr. Turok: One of the, I think, nice things about the study is "The New England Journal" publishes papers that change practice. That is their main motivator for selecting research articles. And you have a very low chance of submitting something and getting it published. But it was very reassuring to know that they felt this was important enough to be published there and that they were confident that it would change practice.
And there are lots of other organizations, professional organizations, a variety of health practitioners, and providers that can disseminate this to people who work with them.
I also have been working with the people from UpToDate to revise the article on emergency contraception to incorporate this and they were amazing. ACOG carried a piece on their listserv email and we're going to work with them to try to update Lark information in their emergency contraception information. So there are all kinds of ways to get the information out.
And a really important place to do that is also with Planned Parenthood Federation of America. As you know, they have something called the National Medical Committee that makes decisions on changes in practice. So I just sent an email and lately before this interview responding to questions from people who organize the National Medical Committee about this.
It's, I think, a great opportunity for Planned Parenthood Federation of America to lead on the dissemination of this because the information came exclusively from Planned Parenthood clinics. This is a collaboration between our team at the University of Utah and Planned Parenthood Association of Utah.
If you look at what gets published in "The New England Journal," the vast majority . . . and currently, probably nobody is a more fastidious reader and consumer of their publication than you. If you look at those trials that get published, most of them are these big, multi-site, and sometimes multinational studies with tons of sites and huge numbers of participants. This study is different.
Dr. Jones: It is. It's really amazing that you have a very local group who was completely committed to answering the question. And I think that that's a phenomenal thing.
I think, at The Scope, we're trying to get the word out also to individual women so they might be willing to come in and ask. So not only do clinicians need to know, but if individual women say, "By the way, do you think I could get this IUD today? Do I have to wait?" that changes practice.
Dr. Turok: Absolutely. So the education and dissemination of information have to be from push and pull factors from supply and demand side. And as I had mentioned, we're already working on trying to get providers up to speed. But there's lots of opportunity that we're going to be working on to make sure that people who are seeking emergency contraception will know about this.
Obviously, the internet is a fabulous place to do that. And there are also some organizations that focus specifically on emergency contraception. There's a U.S. Emergency Contraception Consortium and an International Consortium of Emergency Contraception, and they are fabulous at providing consumers information about different products and ways to access them. So we look forward to working with them as well.
Dr. Jones: Right. Well, Dr. Turok, I am very grateful for your time, and we'll work at The Scope in trying to get people the information they need. But the research to answer this kind of question takes years and takes a team of dozens of nurses, and clinic staff, and researchers, and above all, it takes hundreds of women who are willing to participate, answer questions, and follow up. To all of them, we are very grateful because "I hope I just didn't get pregnant" isn't a very good birth control method. And it's been a long time coming and I'm so glad to see it here. Thanks a lot, and thanks for joining us on The Scope.