![[media-entity-reference:media-alt]](/sites/g/files/zrelqx136/files/styles/billboard_tablet/public/media/images/2021/vasectomy-reversal.jpg?h=e066b8dd&itok=C_53Mlj6)
![[media-entity-reference:media-alt]](/sites/g/files/zrelqx136/files/styles/billboard_desktop/public/media/images/2021/vasectomy-reversal.jpg?h=e066b8dd&itok=vGY0PHyR)
Fertility Treatments for Men
Getting an accurate and complete diagnosis helps couples dealing with infertility find the best treatment method. University of Utah Health's Andrology Lab provides both common and more advanced fertility testing procedures that other facilities don't provide.
Infertility treatment is one of the fastest advancing fields in medical science. As an academic medical center, University of Utah Health’s andrology lab is a leader in bringing our patients the latest advancements in infertility testing.
Find a Fertility Specialist
Semen Analysis
Semen analysis is the most efficient and inexpensive way to study male fertility. It’s usually the starting point for a male infertility evaluation. Semen analysis checks certain characteristics of your sperm:
- Sperm concentration—how many sperm are in each milliliter of your semen
- A motile sperm count—how well your sperm move and swim
- A progressive motile count—how many sperm are swimming forward
- Morphology—your sperm’s shape
The most important number is the total progressive sperm count. This measures how much sperm moves towards an egg—in other words, how much sperm is available to fertilize an egg.
The shape of your sperm is also somewhat important, although male infertility researchers have yet to determine how important.
A normal semen sample is usually made of 35% normal, correctly shaped sperm. The other 65% of sperm are often abnormally shaped or abnormal. A low percentage of normal sperm could cause infertility problems.
Anti-Sperm Antibody Test
Your body’s immune system attacks anything that has different DNA than your own. The genetic material in each sperm is different from the man who makes them. So, all men have barriers that protect their sperm from their body’s immune system. These barriers help keep your body from identifying your sperm as foreign or dangerous.
Your body produces antibodies to attack your sperm when these barriers break down. These antibodies may attach themselves to your sperm, which can damage your sperm’s ability to move or clump with other cells.
We sometimes test for antibodies by evaluating seminal fluid, semen, and the serum from the woman. You should have an anti-sperm antibody evaluation if the following applies to you:
- Your sperm motility (movement) is low when you’re getting ready for a vasectomy reversal.
- You have a higher amount of antibodies.
- Your sperm may not work correctly.
Women may also produce anti-sperm antibodies. Women should get a test for anti-sperm antibodies if a sperm cervical mucus interaction assay test suggests a problem.
Retrograde Semen Analysis
We may recommend a retrograde semen analysis for men with a low sperm count. (An initial semen analysis will show if you have a low sperm count). Retrograde ejaculation is when sperm ends up in your urine after you have sex. Retrograde ejaculation is not dangerous but can impact a man’s fertility. Many men with retrograde ejaculation have had an earlier surgery or medical condition that makes them more likely to develop retrograde ejaculation.
The following conditions can make you more likely to develop retrograde ejaculation:
- Testicular cancer surgery (RPLND)
- Transurethral surgery of the prostate
- Childhood bladder surgery
- Diabetes
- MS
- Spinal cord injury
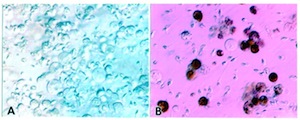
Sperm Chromatin Integrity Test (SCIT)
An SCIT test (also known as DNA fragmentation test) analyzes the quality of your chromatin and whether there are any breaks in your DNA strands. Chromatin is a bundle of genetic material inside your cells and includes DNA, RNA, and protein. All of these things affect an embryo’s quality.
Your body usually repairs any broken DNA strands at the end of sperm production. But sometimes your body doesn't repair any DNA damage. If it doesn’t, your sperm may struggle to fertilize an egg or affect an embryo’s quality. The SCIT test allows us to see if damage to your sperm causes infertility.

