Dr. Miller: MS or multiple sclerosis. What is it and what can you do about it? We're going to talk about that next on Scope Radio. This is Dr. Tom Miller.
Announcer: Medical news and research from University of Utah physicians and specialists you can use for a happier and healthier life. You're listening to The Scope.
Dr. Miller: I'm here today with Dr. Dana Dewitt who is a professor of neurology and a specialist in multiple sclerosis care. Dana, what is multiple sclerosis? I think we've heard the term but what is it and how does it present and when should somebody be concerned that they might have it?
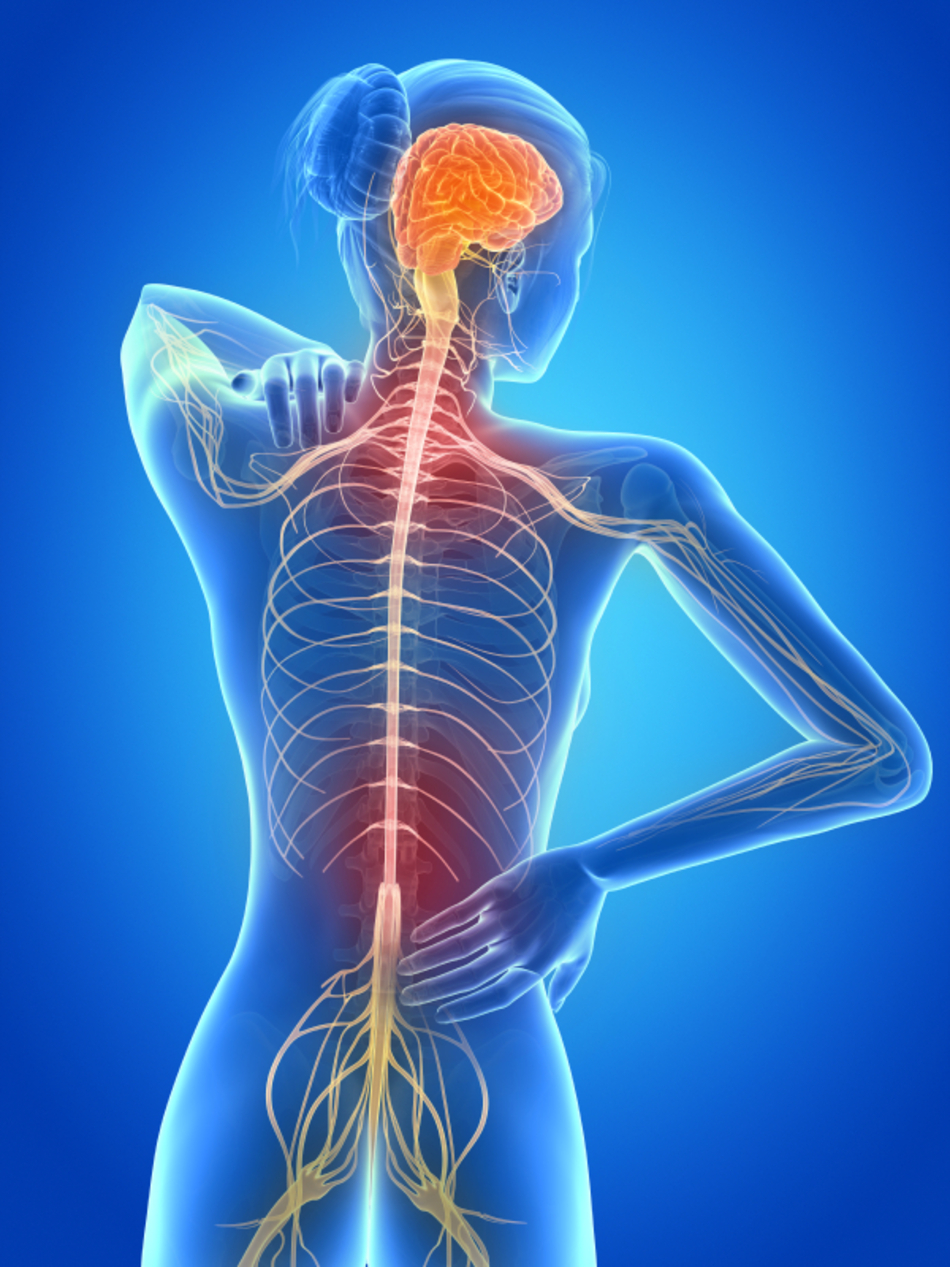
Dr. Dewitt: Everybody seems to know about the term "multiple sclerosis," but many people really don't understand what it is. It's certainly a neurologic disease. It is a disease that occurs because the immune system is activated and attacks the myelin in the brain and the spinal chord.
Dr. Miller: And we don't know why that occurs, is that true?
Dr. Dewitt: We don't know why that occurs. We know that there's a genetic input. We know that it may have something to do with Vitamin D levels, but we also don't know what actually is the spark that sets it off.
Dr. Miller: So if it's "set off," what does one experience? What are some of the symptoms that might arise?
Dr. Dewitt: There are some classic symptoms with MS. The attack on the nervous system can be on the optic nerve and can cause something that we call "optic neuritis."
Dr. Miller: Which changes vision, I guess?
Dr. Dewitt: Which changes vision. It causes, sometimes, a painful, kind of gritty feeling in the eye and then dimming of vision over time in one eye. The other thing that can happen is that the spinal chord can be attacked and you can end up with numbness or weakness of an arm and a leg or both legs, bladder and bowel dysfunction. Other parts of the brain can be affected that can cause double vision, vertigo, imbalance, those kinds of things.
Dr. Miller: But sometimes it can come on subtly. I mean, I've had a patient in the past who developed multiple sclerosis. His first time was running. He couldn't quite run as far. He had a weakness in one of the legs and then that sort of progressed.
Dr. Dewitt: That's true and there are different forms of MS, the most common type being relapsing/remitting disease. The beginning symptom can sometimes come on over days or a week or two and just get worse and worse. The interesting thing with relapsing/remitting disease is the nervous system has a way of healing itself in MS and so sometimes the symptoms get better and the patient ends up not coming to the attention of a physician early enough, until they've had a few events. At that point, we discover that they've probably had MS for a few years.
Dr. Miller: Now you can have numbness, I guess, on one leg or arm and then maybe weakness on the other and it could alternate back and forth. It could have some sort of strange presentations I think, is that right?
Dr. Dewitt: Exactly and you can have different things occur at different times.
Dr. Miller: Presenting with some of the symptoms that you've just talked about, how do you make the diagnosis and then what do we do about it?
Dr. Dewitt: Probably referral to a neurologist who would listen to your symptoms and do a complete neurologic exam to see what they think is happening. Then one of the ways MS is diagnosed is with an MRI scan and MRI is very, very good at showing the what we call plaque-like lesions that can occur in MS.
Dr. Miller: These little spots on the brain that are tell-tale signs of multiple sclerosis.
Dr. Dewitt: Exactly.
Dr. Miller: So does that mean that we don't have to do this lumbar puncture anymore, to take spinal fluid out and look at it under the microscope?
Most of the time I like doing a lumbar puncture. It tells me how much inflammation there is. It rules out what we call MS mimickers or other unusual things that can look like MS. If an MRI is absolutely classic for MS, occasionally, a lumbar puncture might not be necessary.
Dr. Miller: So you might still need that?
Dr. Dewitt: Yes.
Dr. Miller: Okay. Now, in the not-too-distant past the main treatment was steroids prednisone but there are a lot of new treatments now.
Dr. Dewitt: Most of the initial FDA treatments actually date back to about 1995. So, we've had treatments for quite some time. The major treatments are an interferon or something called glatiramer acetate. Those are all given by injections, which has been a bit problematic for some patients along the way, but they are very effective. They've been around so long we know what to expect and we know how safe they are and they really work. What's been shown in clinical trials is that getting on the drug early and staying on the drug makes an enormous amount of difference.
Now, we do have three new FDA approved oral agents that become options as well. So, the whole armamentarium of treatment for MS now has grown enormously. We still know the important thing is being diagnosed early, getting on treatment, staying on treatment.
Dr. Miller: What looks great in the future? Do you see any treatments on the horizon that you're excited about?
Dr. Dewitt: Well, we're hoping. We're actually doing a clinical trial here now for a new treatment for secondary progressive and what's called primary progressive MS, which are two different presentations for MS different from relapsing/remitting disease. And there really have not been good treatments for those forms of the disease. So we're very excited that we're actually doing this clinical trial here to look at this agent.
I think the other developments are there are a couple of clinical trials looking at potential remyelinating type agents where damage that has occurred in the past can actually be repaired and I think that's what we really want more than anything. The other thing is we're learning more and more with MRI in that we're able to do special MRIs looking at brain volume and we're able to look at certain agents to see if we can prevent degeneration and progression of disease in different ways than what we have available now.
Dr. Miller: You know, it's interesting. With the advent of MRI, which is a magnetic way of looking at the brain. That's allowed this field to progress in its ability to treat people, I think, because now you can actually see inside the brain on these images and look at the plaques and sort of figure out if there are more of them or if they're growing, right? So that's been key.
Dr. Dewitt: Exactly. It's been huge. Part of it is that once a plaque forms it will stay on the MRI as a scar and so we can differentiate between old lesions, new lesions, lesions that enhance with contrast agents. And now we're able to do these brain volume measurements to see how well some of the new medications are working to prevent progression.
Dr. Miller: This allows us a way to really see if the drugs are working and treatment's working. I had heard that stem cell transplant or bone marrow transplant was being tried in the past. Has that been effective at all?
Dr. Dewitt: Yes, there are some places where there are still clinical trials and there are places where bone marrow transplants are being done. There are different kinds of bone marrow transplants. The traditional bone marrow transplant where patients are given high-dose chemotherapy to totally eradicate the bone marrow. The question has always remained in those cases whether the high-dose chemotherapy actually treated the disease effectively enough that it's not really the bone marrow transplant, but those questions are still up in the air.
There are other types of bone marrow transplants now. Something called a mesenchymal transplant or multi-stem, which are these actual intravenous infusions which is a different kind of mode of stem cell transplant which, I think, is the major excitement for the future because I think they're going to turn out to be immune regulators that are far safer than the traditional way of doing a stem cell transplant.
Dr. Miller: Now treating multiple sclerosis is one of your areas of expertise. Would you recommend that people with multiple sclerosis seek a neurologist who have experience with multiple sclerosis?
Dr. Dewitt: I strongly do for a couple of reasons. One is I think making the diagnosis is important and sometimes it can be not so clear. So I think you need a specialist to make the diagnosis. The second thing is now that we have so many treatments, it's important for someone with experience who follows a lot of these patients to be able to choose the proper treatment for you, monitor you to know whether you're responding to that treatment, and then decide whether you need to be changed to something else and follow you over time and just see how you're doing.
Dr. Miller: So it sounds to me like early diagnosis, early treatment, and rigorous follow-up by a specialist who's an expert in multiple sclerosis can make a great difference in the health of these patients.
Dr. Dewitt: Exactly.
Dr. Miller: Any final thoughts?
Dr. Dewitt: We have so many developments for treating MS that it's changed the scope of the disease. It's always hard to give someone the diagnosis at the beginning because people do have a preset idea of what it means and they look down the road and they're very worried about having a chronic condition. I think what I'd like to say is that the treatments that we have available now are really excellent treatments and as long you're followed closely and you know you're on a medication that works, most people with MS live an absolutely normal life.
Announcer: We're your daily dose of science, conversation, medicine. This is The Scope. University of Utah Health Sciences radio.


