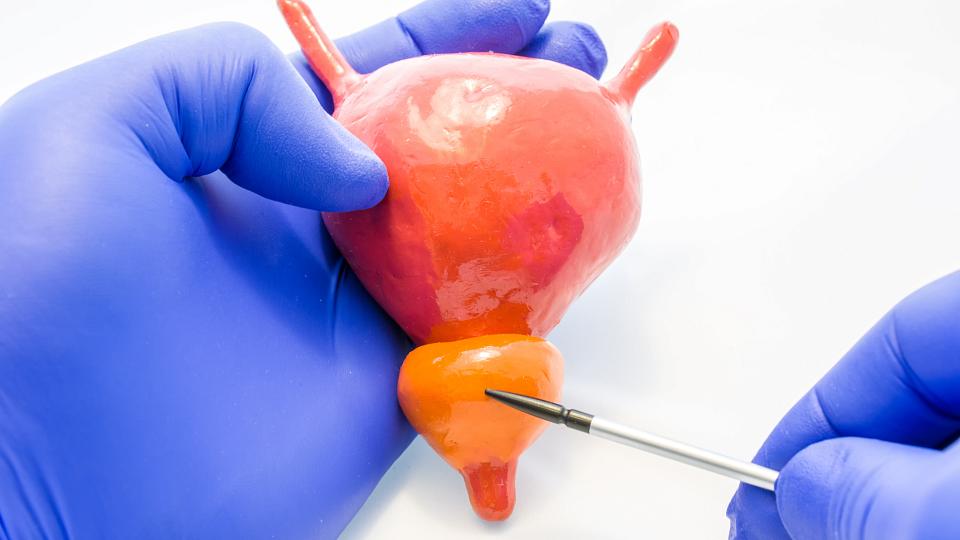
What Is the Prostate?
The prostate is a male gland. It surrounds the urethra (urinary channel) that connects to the bladder. During a male’s fertile years, the prostate gland makes fluid that comes out during ejaculation. As men get older, their prostate may become enlarged. Most men will experience some prostate growth starting in their 30s. However, symptoms may not be noticeable until age 50 or later.
At University of Utah Health, our urologists provide the full spectrum of treatment for men with an enlarged prostate — also known as benign prostatic hyperplasia (BPH). Our highly trained specialists help diagnose enlarged prostate issues and offer a range of treatments, including conservative treatments, minimally invasive surgery options, and more advanced surgeries.
What Is the Normal Size of the Prostate Gland?
A normal-sized prostate is around 25 grams — approximately the size of a walnut. However, an enlarged prostate may grow well over three times the normal size (over 80 grams). The size of a man’s prostate varies from person to person. Size is just one of the many factors we consider when determining whether a man needs treatment for BPH.
Our doctors use a variety of tools to determine if you have an enlarged prostate and need treatment, including:
- physical examination,
- symptom discussion,
- severity of symptoms,
- diagnostic tests, and
- laboratory tests.
Prostate Enlargement Symptoms
The most common symptoms of BPH (enlarged prostate) relate to urinary function. You may experience:
- bladder obstruction, such as a slow stream of urine;
- starting and stopping while urinating;
- inability to empty your bladder completely;
- bladder irritation or discomfort;
- feeling an urgency to urinate;
- waking up multiple times at night to urinate; or
- urinary incontinence (an inability to control your bladder).
When you work harder to push urine out, these urinary symptoms could eventually put pressure on your bladder. This may lead to bladder abnormalities or other issues. It’s important to discuss any potential symptoms of BPH with your doctor.
When to See a Doctor
About half of all men over the age of 40 will experience some symptoms of BPH. If these symptoms become bothersome or interfere with your daily life, talk to your primary care provider or schedule an appointment to see a urology specialist. Ignoring your symptoms could lead to even more discomfort and disruption in your life. In severe cases, an enlarged prostate could lead to bladder or kidney problems if left untreated.
This is a modal window.
Enlarged Prostate Causes
The exact cause of BPH (enlarged prostate) is not known. Most men will experience prostate enlargement as they get older. Some risk factors that could contribute to prostate enlargement include:
- family history of enlarged prostate,
- being overweight or obese,
- living a sedentary lifestyle,
- diabetes,
- heart disease, and
- aging.
The following items don’t cause BPH, but could make your symptoms worse, including:
- certain prescription medications, such as beta blockers and diuretics;
- a class of antidepressants called tricyclic antidepressants;
- over-the-counter medications such as antihistamines, decongestants, or NSAIDs (non-steroidal anti-inflammatory drugs);
- some types of beverages, such as alcohol, coffee, tea, or soda; and
- certain foods, such as red meat, spicy foods, or dairy.
Find a Urologist
Scott A. Hopkins, MD
How Is an Enlarged Prostate Diagnosed?
A primary care provider (PCP) or urologist will diagnose BPH (enlarged prostate) after a discussion of your symptoms and a physical exam. Your doctor may recommend additional tests or imaging if the cause is not clear or if they need to rule out other conditions. The specific tests you need, if any, will depend on your health, family history, and other factors.
These tests may include:
- Urine test
- Digital rectal exam — The doctor will use their finger to determine the prostate size and texture.
- Blood tests — These will help identify or rule out any kidney problems.
- PSA blood test — This test will identify any levels of prostate-specific antigen (PSA) in your blood, a chemical made by the prostate.
- Urinary flow test — This test will measure your urine volume and strength of the flow.
- Voiding diary — This journal will help you keep track of how often and how much you urinate in 24 hours.
- Transrectal ultrasound — We will insert a probe into your rectum that sends out high-energy sound waves to visualize and measure the size of your prostate.
- Urodynamic (pressure flow) study — During this study, a catheter (long, thin tube) will be inserted in your urethra.
- Cystoscopy — We will use a camera to view your urethra and bladder.
Enlarged Prostate Treatment
There are several treatment options for BPH (enlarged prostate).
Watchful Waiting
If you have minimal symptoms, your urologist may recommend a period of “watchful waiting.” You may be instructed to make some changes to your diet and lifestyle habits to relieve symptoms of BPH, such as losing weight (if necessary) or controlling your blood sugar levels. Your doctor may also encourage you to keep a diary about your symptoms to see if they worsen over time.
Our doctors will schedule your appointments at regular intervals (at least once a year or more often, if necessary) to:
- Discuss your symptoms.
- Conduct a physical exam.
- Order lab tests.
If your BPH gets worse, your doctor will recommend one or more of the following treatment options.
Medications
Some patients can successfully address BPH with medication and avoid the need for surgery or other interventions. There are four common medications we prescribe for an enlarged prostate, either on their own or in combination with one another:
- Alpha blockers — This medication will relax your prostate and bladder opening to allow better urine flow. Many people see an improvement in their symptoms without serious side effects.
- 5-alpha reductase inhibitors — This medication will block hormones that can lead to prostrate growth. As a result, your prostate will shrink slowly over a period of four to six months. This medication works best for patients with significant prostate enlargement.
- Anticholinergic medications — This medication will block receptors in your nerve cells that cause muscle movement in the gastrointestinal tract. It treats overactive bladder, frequent urination, and consistent urges to urinate.
- PDE5 inhibitors — This medication will relax the muscles in your bladder and prostate to reduce some of the symptoms of BPH.
Enlarged Prostate Surgery
If medications do not work to reduce or eliminate symptoms of BPH, your urologist may recommend prostate surgery. Our urologists perform a wide range of surgeries to open the urethra where it runs through the prostate.
Can an Enlarged Prostate Be Cured?
For most patients, BPH (enlarged prostate) is curable. Some people see a significant reduction in symptoms with medication alone. If medicine does not work, or your prostate is too large, surgery will often remove enough of the prostate to provide you with relief. However, there is a chance that your prostate tissue will grow back. If that occurs, your doctor may recommend additional surgery or medication.
This is a modal window.
Is an Enlarged Prostate Cancerous?
Benign prostatic hyperplasia means that you are experiencing abnormal cell growth in your prostate, which causes it to get larger. Benign means it is not cancer. Studies have found no link between BPH and prostate cancer. In fact, an enlarged prostate will not increase your risk for developing prostate cancer.
If your urologist suspects that you might have prostate cancer, he or she will recommend diagnostic tests, such as:
- a prostate biopsy,
- PSA test (prostate-specific antigen, a chemical made by the prostate), or
- prostate MRI.
Some late-stage cancers may also show symptoms that are similar to an enlarged prostate, especially if your cancer is in the area of your urethra. Talk to your doctor about your symptoms to get a proper diagnosis.
This is a modal window.
Natural Remedies for Enlarged Prostate
Most natural remedies have little or no scientific research to indicate whether they are effective for treating the symptoms of BPH (enlarged prostate).
However, you can reduce the symptoms of BPH by:
- eating a healthy diet.
- eating five servings of fruits and vegetables each day (especially citrus fruits).
- doing moderate to vigorous exercise on most days.
- losing weight or maintaining a healthy body weight.
- limiting caffeine and alcohol (they can increase the urge to urinate).
- avoiding liquids a few hours before bed.
Foods and Beverages to Avoid with Enlarged Prostate
Some foods and beverages may negatively impact the health of your prostate or worsen your BPH symptoms. The types of foods that might irritate your bladder can vary from person to person, so some foods might not affect you while others do.
Discuss with your doctor which of these "bladder irritants" you may want to avoid:
- caffeine,
- alcohol,
- red meat,
- processed meat,
- high-fat foods (such as dairy),
- chocolate,
- tomatoes, and/or
- acidic fruits (such as grapefruits, lemons, and oranges).
This is a modal window.
Schedule an Appointment to See a Urologist
Call U of U Health Urology at 801-213-2700 to schedule an appointment with one of our experienced urologists.
You do not need a referral from your PCP to schedule an appointment with us. However, some insurance providers require that you get a referral before you see a specialist. Contact your insurance carrier with any questions you may have about your plan requirements.
Our Specialists in the Media
This is a modal window.
This is a modal window.