Dr. Miller: Thin bones and the risk of fracture and what to do about that. We're going to talk about that next on Scope Radio.
Announcer: Health tips, medical news, research, and more for a happier, healthier life. From University of Utah Health Sciences, this is The Scope.
Causes of Thin Bone Fractures
Dr. Miller: I'm Dr. Tom Miller and I'm here with Dr. Nick Spina, and he's an orthopedic surgeon here at the University of Utah, in the Department of Orthopedics. He's an expert in spine care. Nick, how do you get a fracture when you have thin bones or osteoporosis? What happens? Where do they occur typically in the back? Tell me about that. It's a lot at risk.
Aging
Dr. Spina: Yeah. Osteoporotic compression fractures or what we call fragility fractures are probably the most common fracture we see in spine surgery. It tends to be on the more elderly side of the population.
Dr. Miller: At the time when we lose our bone mass.
Osteoporosis
Dr. Spina: Exactly, at the time when we lose our bone mass. So I'd like to describe them to people to imagine a soda can or a pop can. And each patient's vertebral body is like a pop can. So it has a hard rim on the top and a hard rim on the bottom, and the center part of the can is relatively empty. As we age and we get osteoporosis, the center of the can becomes even more empty. And so, as we stress the top, the can eventually cracks and crushes where our end plates become closer together or the ends of the can become closer together.
Activities That Can Cause Fragility Fractures
Dr. Miller: And so, what happens to precipitate that fracture? My understanding is they could just happen spontaneously if your bone density is so low.
Your Bone Strength Determines A Lot
Dr. Spina: Right. Depending on the degree of your osteoporosis or the degree of the strength of your bone, it can happen with just minimal activities such as waking up from sleep, standing, walking. They are commonly precipitated from falls, so patients often come in after a fall from standing or a fall during gardening, or routine activity around the house where they develop an acute onset of back pain.
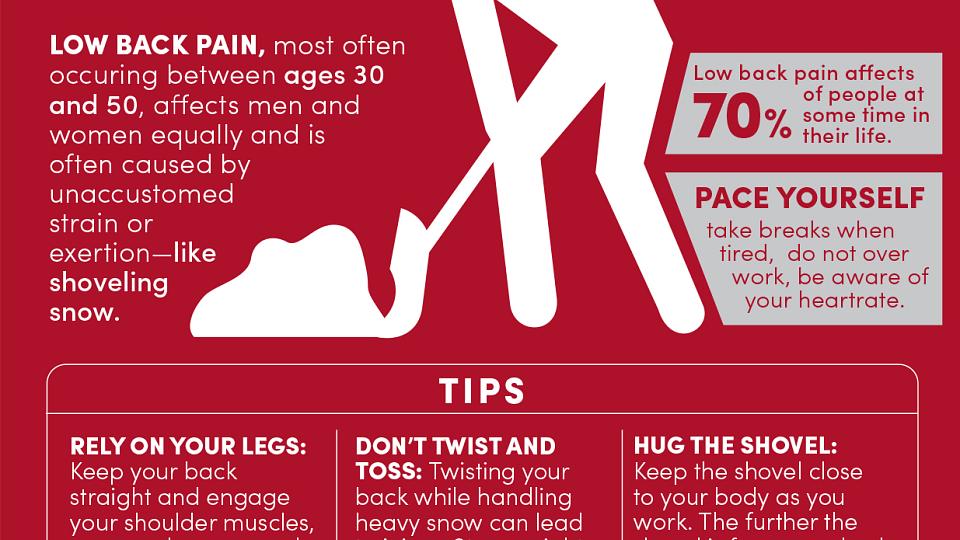
Dr. Miller: Or one of the favorites from my patients would be shoveling snow.
Dr. Spina: Exactly. It seems no one should shovel snow anymore. That's pretty much a general rule.
Dr. Miller: So what happens? Do they have pain typically after that?
Fracture Symptoms
Dr. Spina: So the most common presenting symptom is acute back pain. Some of the worst pain you've had in the center of your back. It tends to be localized to the midline or right in the middle. Our muscles also become very inflamed, so it can radiate out towards our rib cage. It tends to be in the mid portion of the back. For women, right around their bra strap, and for men, kind of in-between the shoulder blades.
Osteoporosis in Women vs. Men
Dr. Miller: Now, you would find more osteoporotic fractures in women, I would think, right?
Dr. Spina: It does.
Dr. Miller: Osteoporosis is more common in women.
Dr. Spina: It's more common in women. So we do tend to see more osteoporotic fractures in elderly women versus men.
Treatment Options
Dr. Miller: So, aside from analgesics, pain killers, that type of thing, what can you do to alleviate the pain or help with the pain?
Activity Modification
Dr. Spina: So we sort of take a two-tier approach. One is a reduction in activities and modification of daily living, to avoid those activities such as heavy lifting, bending over at the waist, stressing the spine by bending forward or twisting. And the second would be we occasionally use a brace to provide an external support, kind of external crutch you can think of to keep the spine upright or support it while a bone tends to heal in that compressed manner.
Back Bracing
Dr. Miller: What's this brace look like? Is it corset?
Dr. Spina: Yes. It tends to be a corset. It kind of looks like a turtle shell, hard in the front and hard in the back, and it wraps around your torso.
Dr. Miller: And usually, how long would a person have to wear that for that to work?
Dr. Spina: We tend to use them for about two months. And then, we tend to wean out of it because as we put people in braces, their muscles, obviously, become weaker. And having good muscular strength is one of the ways we compensate for having fractures. And so we don't cut them cold turkey. We often ask people to slowly come out of them and wear them when they're upright or up for long periods of time, and then remove them when they're sleeping or sitting.
Kyphoplasty and Vertebroplasty
Dr. Miller: Now, tell me a little bit about what's call kyphoplasty. I understand there's a little bit of controversy about the use of this technique and has been for a number of years.
Dr. Spina: So kyphoplasty and vertebroplasty were very common about 10 to 15 years ago. They sort of exploded in the world of spine surgery. And the procedure itself is directed at restoring the height of that pop can. So what we do is . . .
Dr. Miller: So this maintains height in the patient. So the concept, I guess, was if you increase the height of the crushed pop can, then the person wouldn't lose height.
How It's Done
Dr. Spina: Exactly. And so we insert a probe from the back of the spine into the front, the vertebral body. And there are two different means. One, we use a balloon to try to restore the height of the body. And the second is we just inject a material to try to restore the height. And the bottom line is that we take the empty space in the vertebral body, that space that's crushed down, and we try to stabilize it and if not, restore it by putting cement in the front of the vertebral body.
The Controversy
Dr. Miller: So what is the controversy surrounding this technique?
Dr. Spina: So there have been a couple large studies that have been done, that have looked at patients who have not had vertebroplasty or kyphoplasty and who have, and they haven't shown much of a difference as far as long term outcomes. So, in my practice, we tend to reserve them for those patients with intractable pain after about six weeks of non-operative care.
Potential Benefits
Dr. Miller: So they have some role in alleviating pain if it's not treated with the standard sort of non-interventional means that you just spoke about a few minutes ago?
Dr. Spina: Exactly. In those patients out of refractory which are very, very few in my practice, tend to see a little bit of benefit from doing a kyphoplasty. But again, we tend to reserve that to those people that fail all the non-operative means which we start with in the beginning.
Osteoporosis Medications
Dr. Miller: The other point would be that if a patient has osteoporosis, they should also be treated for that with one of the newer medications. I should say newer. The medications have been around now for 10 years, and there's new medicines coming out all the time.
The Importance of Osteoporosis Screenings
Dr. Spina: Exactly. One of the biggest risk factors for vertebral body compression fracture or fragility fracture is having a previous fracture. So it's our routine practice when we identify these patients to make sure that they have a pipeline of care through either us as treating providers or their primary care physicians to check their bone quality through a DEXA scan and address the degree of osteoporosis that they have.
Dr. Miller: Screening becomes very important in this age group, especially women over 65 years of age.
Dr. Spina: Exactly. Screening is probably the best form of prevention for these fractures that we have.
Announcer: Want The Scope delivered straight to your inbox? Enter your email address at thescoperadio.com and click "Sign Me Up" for updates of our latest episodes. The Scope Radio is a production of University of Utah Health Sciences.