What Is the Difference Between Type 1 & Type 2 Diabetes?
Type 2 diabetes is the most common kind of diabetes. Lifestyle factors such as diet and exercise, genetics, and some medications can cause you to develop the condition. It’s sometimes called adult-onset diabetes. Type 2 diabetes occurs when your body doesn’t make enough insulin or doesn’t use it well. Insulin, a hormone made by the pancreas, turns the sugar (glucose) in your food into energy for your body. If there isn’t enough insulin to process the sugar in your cells, it stays in your blood, causing diabetes.
Type 1 diabetes occurs when your immune system destroys cells in your pancreas that make insulin. Therefore, you have very little or no insulin in your body. Providers usually diagnose children and young adults with type 1 diabetes, but it can appear at any age.
Find a Diabetes Specialist
Type 2 Diabetes Symptoms
Symptoms of type 2 diabetes can be different for each person. Type 2 diabetes can be hard to detect because some people don’t have any symptoms. Other people have only barely noticeable and mild symptoms. In the US, half of people with diabetes don’t even know they have it.
People can also mistake symptoms of type 2 diabetes for other health problems. Be sure to see your provider for a correct diagnosis. If you experience any of these symptoms, see your doctor about getting your blood sugar tested:
- Blurry vision
- Dry, itchy skin
- Excessive thirst
- Frequent bladder infections or skin infections that take a long time to heal
- Irritability and mood changes
- Nausea or vomiting
- Numbness or tingling in your hands and feet
- Unexplained weight loss even though you’re hungrier than usual
- Urinating (peeing) frequently
- Weakness and fatigue
What Causes Type 2 Diabetes?
Specialists and researchers don’t know exactly why type 2 diabetes occurs. Some families have higher rates of the disease. But lifestyle factors like poor diet, obesity, and not exercising enough increase your chances of developing the disease. Prolonged use of steroids and other medications may also increase your risk.
Type 2 Diabetes Risk Factors
- Age over 45 years old
- Being overweight
- Family history of diabetes
- High triglycerides
- Infrequent exercise
- Low high-density lipoprotein (HDL), also known as the “good cholesterol”
- Developing gestational diabetes during pregnancy
- Race and ethnicity, including Black, Hispanic, Native American and Asian people, and Pacific Islanders
- Smoking
Type 2 Diabetes Complications
Type 2 diabetes can lead to serious health problems if you don’t get treatment or follow your provider’s recommendations to manage it:
- Blood flow—High glucose levels cause fatty deposits in your blood vessels that slow blood flow through your body.
- Eyes—Diabetes puts you at risk for diabetic retinopathy, macular swelling, cataracts, and glaucoma.
- Feet and legs—High blood sugar can cause a host of problems with your lower extremities, including nerve damage, wounds that are slow to heal, swelling, and dry, cracked skin.
- Heart—Too much sugar in your blood damages your heart’s blood vessels and nerves. You’re at higher risk of heart disease, high blood pressure, and coronary artery disease.
- Kidneys—Diabetes damages your kidneys’ ability to filter water and toxins from your blood.
- Nerves—People with diabetes are at higher risk of peripheral neuropathy, a condition causes pain and numbness in your hands and feet.
Over time, health problems in these parts of your body can cause kidney failure, blindness, stroke, gangrene, or the need for amputation.
How to Test for Type 2 Diabetes
Specialists use a variety of tests to diagnose type 2 diabetes:
- Hemoglobin A1C—This test measures your average blood sugar levels during the last 2–3 months. If your A1C is more than 6.5%, you have diabetes.
- Fasting glucose—Fasting glucose checks your blood sugar levels after you haven’t eaten for eight hours (called fasting). Most people take this test before eating their first meal of the day. Specialists call this test your fasting blood glucose level. If your fasting blood glucose is higher than or equal to 126 milligrams per deciliter (mg/dl), you have type 2 diabetes.
- Oral glucose tolerance test (OGTT)—Specialists measure your blood sugar level before and two hours after you have a sugary drink. The OGTT lets your provider know how well your body uses glucose. If your blood sugar level is 200 mg/dl or more two hours after the sugary drink, you have type 2 diabetes.
- Random glucose test—Providers can give you a random glucose test at any time of the day. If your blood sugar level is 200 mg/dl or more, and if you have symptoms of high blood sugar, you have type 2 diabetes.
It’s best to take the tests a second time to confirm your diagnosis.
Type 2 Diabetes Treatment
The goal of diabetes treatment is to keep your sugar levels in check. It’s important your blood sugar levels don’t dip too low or become too high. To keep blood sugar as level as possible, you will need to eat a healthy diet, exercise regularly, and get regular check-ups.
Providers consider several factors about your life when treating type 2 diabetes:
- Your age
- Your overall health and health history
- Your reaction to medications, procedures, or treatments
- Your opinions and preferences about treatment
It’s important to stay in contact with your provider if you have trouble managing your blood sugar or if you notice trends. For example, see your provider if you have high blood sugar levels throughout the day, if you find your blood sugar level is always high at the same time of the day, or if you are having symptoms of high blood sugar like drinking or urinating more than normal.
Type 2 Diabetes Medications
Some people can control their type 2 diabetes without medication by losing weight, exercising regularly, and eating a healthy diet. Other people will need to take oral or injection medications like insulin or newer medicines that increase your insulin.
Several medicines can treat type 2 diabetes, including many kinds of oral medications (usually pills). Each type works in a different way to lower blood sugar. Some providers recommend patients combine medications to control their blood sugar better.
Type 2 Diabetes Diet
You and your provider can develop a meal plan to control your diabetes. Some people need to eat meals and snacks at the same time every day. Other people find eating several small meals throughout the day manages their symptoms.
Eating a range of healthy foods from every food group is key. In general, specialists recommend you limit certain foods and drinks:
- Avoid added sugars, like juice, sugary soda or energy drinks, cookies, candy, and ice cream.
- Avoid high levels of salt, saturated fat, or trans fat.
- Avoid high levels of low-fiber starches, like white bread, pasta, and rice.
Talk to your provider if you have questions about using certain diets such as the ketogenic (keto) diet, paleo diet, or veganism to manage your diabetes.
Exercise and Diabetes
Exercise plays an important role in managing type 2 diabetes. Be sure to get at least 150 minutes of exercise each week. Don’t let more than two days go by without exercising. If you sit for long amounts of time, be sure to stand up every 30 minutes and get some light activity.
Type 2 Diabetes Monitoring Guidelines
Specialists recommend that people with type 2 diabetes test their hemoglobin A1C levels at least once every six months if they have stable blood sugar levels in a healthy range. If your blood sugar level is unstable, you should check your A1C levels more often.
Can Type 2 Diabetes Be Reversed?
You can sometimes reverse mild type 2 diabetes with intensive lifestyle changes and weight loss. Some people with this condition will need to manage it with medication, diet, and exercise for the rest of their lives. Specialists consider diabetes a chronic disease because it’s a long-term health problem that only rarely can be cured or prevented with medication.
How to Prevent Type 2 Diabetes
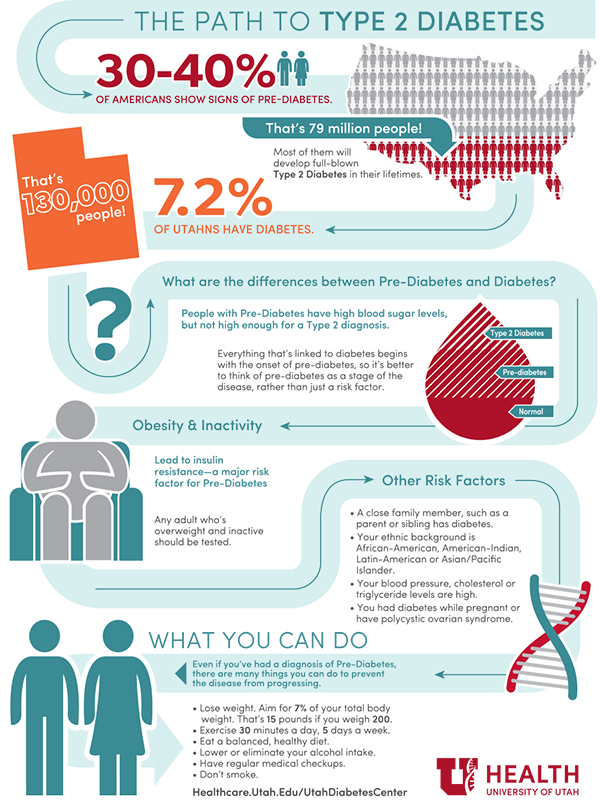
Many people have prediabetes before they develop type 2 diabetes. You may be able to lower your chances of developing type 2 diabetes through lifestyle changes:
- Lose weight. Losing 5–7 percent of your starting weight can reduce your risk for developing diabetes. For example, if you weigh 250 pounds, you should aim to lose between 12.5–17.5 pounds.
- Be active. Getting 30 minutes of physical activity five days a week will reduce your risk. Start slowly and work up to your goal. Talk with your provider before starting an exercise program, especially if you haven’t been active for an extended period.
- Eat healthy foods. Choose smaller portions to limit your calories and select foods with less fat. Avoid sugary beverages in favor of water.
- Talk to your doctor. Some medications can decrease your risk of developing type 2 diabetes.
Schedule an Appointment
Providers at the Utah Diabetes and Endocrinology Center (UDEC) offer complete management of blood sugar levels, the latest diagnostic services, and multidisciplinary services to manage diabetes and its complications. You don’t need a referral to see one of our providers. However, please check with your health insurance company to find out if they require one. Make an appointment by calling 801-581-7761.