Types of Thoracic Aortic Aneurysms

When an aneurysm occurs in the chest (above your diaphragm) it's called a thoracic aortic aneurysm. Thoracic aortic aneurysms are classified based on which part of the aorta is abnormal:
- Aortic root aneurysm—the first part of the aorta as it leaves the heart. This is the portion of the aorta where the coronary arteries that supply the heart muscle come from.
- Ascending aortic aneurysms—this is the straight portion of the aorta between the root and the arch
- Aortic arch aneurysms—this is the part of the aorta that curves around the top of the chest from front to back. This part of the aorta gives off the branches to the head and arms
- Descending aortic aneurysms—this is the part of the aorta after the arch that travels down the back of the chest (near the spine) where the aorta descends towards the diaphragm.
While your primary care physician or a general cardiologist may be able to diagnose a thoracic aortic aneurysm broadly, not all general practitioners or general cardiologists will know the differences between these types of TAAs.
That is why it's important to see a cardiothoracic surgeon or a vascular surgeon who has specialized knowledge and experience with TAAs. This specialist can discuss treatment options and help you manage the disease over time.
Image courtesy of OpenStax College under the creative commons license
Virtual Visits
Our specialists are available to meet virtually with you. Feel free to make an appointment with us.
What Causes TAAs?
Many different things can cause TAAs, but the most common causes include the following:
- Age-related weakening in the aorta that develops over time; people over the age of 65 are at the highest risk of developing this disease.
- Smoking or other tobacco use.
- High blood pressure, which can strain the walls of the aorta.
- Plaque buildup in your arteries that can damage the lining of blood vessels.
- Family history of this disease, which can put a person at risk of an aneurysm at a much younger age.
- Genetic disorders including Marfan syndrome, Loeys-Dietz syndrome, and Ehlers-Danlos syndrome.
This is a modal window.
Diagnosing TAAs
Many patients who have a thoracic aortic aneurysm will not have any noticeable symptoms initially, and depending on the size of the aneurysm, may never experience any symptoms. In fact, for many people the diagnosis of a TAA comes as a result of an imaging study, such as a CT scan, MRI, or echocardiogram, during evaluation for something else.
In some cases these imaging studies may be part of a preventive care plan or regular screening if you have a family member with a history of heart issues. In many cases, however, finding a thoracic aortic aneurysm comes as a surprise, or you may never get a TAA diagnosis before you experience symptoms related to the TAA, at which point it will likely need urgent repair.
If you are diagnosed in advance, generally it’s a radiologist or cardiologist who notices a bulging area somewhere along the aorta. In situations where the bulge is small or not growing very fast, your cardiothoracic specialist may simply recommend monitoring and screening rather than surgery.
In cases where the bulge is large, growing rapidly, or where there are other potential risk factors or indicators that it may burst, your specialist will likely recommend surgery. Each patient should see an aortic specialist to create a personalized treatment plan.
Symptoms of TAAs
For most patients there are no actual symptoms of a thoracic aortic aneurysm, particularly when it is small, which makes it an especially dangerous condition. Not every aneurysm will cause complications, but they often grow over time so even a small one could eventually cause problems.
If you do experience any symptoms early on, they may include:
- Deep or throbbing chest pain,
- Back pain,
- Trouble swallowing or pain when swallowing,
- Shortness of breath, and/or
- Hoarseness or cough.
Since these symptoms are similar to many other conditions, you may not immediately realize you have a TAA and may not look for treatment until it becomes a more serious condition when the aneurysm ruptures or bursts.
If you experience a rupture or an aortic dissection, the symptoms are more severe and require immediate medical attention. These include:
- Sudden, severe chest pain,
- Rapid drop in blood pressure,
- Clammy skin or cold sweat,
- Dizziness or loss of consciousness,
- Difficulty breathing, and/or
- Partial paralysis.
Treatment of Thoracic Aortic Aneursym
Unfortunately many people are unaware that they have this condition until they experience a sudden and potentially life-threatening aortic emergency. Fortunately if you can get treatment quickly, a surgical intervention can often extend your life, even if you don’t catch it really early.
There are two types of surgical interventions for thoracic aortic aneurysms. The treatment plan we may recommend will be based on many factors, including:
- overall health and medical history;
- age;
- size, location, and severity of the aneurysm;
- symptoms you are experiencing; and
- ability to tolerate medications or other therapies.
If your cardiothoracic specialist determines that you do need surgery, it will be either:
- a traditional surgery through an incision (similar to open-heart surgery) or
- a thoracic endovascular aneurysm repair (TEVAR) procedure, which is a minimally invasive repair done from inside your blood vessels.*
Not everyone is a candidate for TEVAR, so it’s important to meet with a specialist to outline a full treatment plan.
Find an Aortic Disease Surgeon
Open Surgical Procedure
An open surgical procedure is similar to open-heart surgery. It usually involves a traditional sternotomy incision and the cardiopulmonary bypass machine. The aortic surgeon will remove the abnormal area of the aorta and replace it with a fabric tube graft.
This type of surgery is most often recommended for TAAs that occur on the aortic root, ascending aorta, and aortic arch. For open surgery for a descending thoracic aortic aneurysm we typically need to use a cardiopulmonary bypass machine but we perform the surgery through a larger incision between the ribs and continuing onto the abdomen.
If you have an open surgery for thoracic aortic aneurysm, you will spend about seven to 10 days in the hospital for recovery and monitoring. But you will be able to get up and move within the first 24 hours.
Your recovery will continue for about two months after you are discharged from the hospital. Once you leave the hospital, you can gradually return to normal day-to-day activities and light exercise (like walking). During this time your aortic surgeon may recommend rehabilitation and other activities to make your recovery as successful as possible.
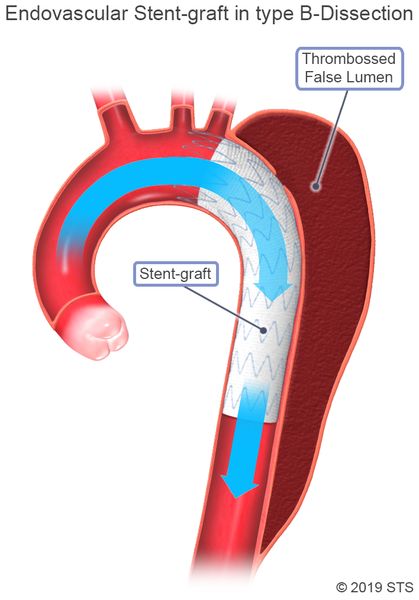
Thoracic Endovascular Aortic Repair (TEVAR)*
Thoracic endovascular aortic repair (TEVAR) surgery may be an option for patients with an aortic arch or descending thoracic aortic aneurysm. Rather than a large incision, we perform this surgery through a series of small incisions, usually in the groin.
In contrast to the open surgical procedure, the abnormal area of the aorta is excluded from the regular pathway for blood flow by placing a stent graft inside the aorta, so blood no longer goes through this damaged area.
While the incision may not be as large, the operation will still take a significant toll on your body and require several days in the hospital for recovery. After surgery you will need up to two months recovery at home before you return to normal daily activities.
During this time your cardiothoracic surgeon may recommend rehabilitation and other activities to make your recovery as successful as possible.
The actual time a you spend in the hospital and in recovery can vary based on many individual factors. Your specialists will work with you to develop a custom plan.
Image courtesy of The Society of Thoracic Surgeons
Non-Surgical Treatment Options
While many patients who experience TAAs will need surgery eventually, there are some situations where you may not. In cases where the aneurysm is small or not growing much, we may recommend regular screenings to watch it over time. This way we can monitor the aneurysm to make sure it doesn’t get worse.
With non-surgical therapies, we work to control blood pressure, sometimes through medication, since higher blood pressure puts stress on the aneurysm. While these therapies and medications are not going to cure the aneurysm, they can slow the progression and possibly surgery.
Not everyone will be a candidate for non-surgical treatment. These options depend entirely on:
- your age,
- size of the TAA at diagnosis,
- family history, and
- other factors.
It’s important to discuss your own situation with your specialist to determine the best treatment course.
Ongoing Treatment, Care, & Follow-up
After surgery, the success rate is different for each patient. It depends on:
- how severe the aneurysm is,
- whether the surgery was performed after an acute event,
- your age and overall health, and
- other factors.
It is important for patients who get surgery to repair a thoracic aortic aneurysm to understand that surgery is not intended to cure the disease, and that TAA is a chronic disease—similar to kidney disease or diabetes—that you will need to monitor and manage for the rest of your life. For most patients that means:
- Regular office visits,
- Regular screenings,
- Monitoring and surveillance with your doctor,
- Medications, and
- Lifestyle changes to reduce the chance of complications.
Schedule a Consultation
Need to see an aortic specialist? First thing to do is get a referral from your primary care doctor. Once you have referral and have made an appointment, you can prepare for your appointment by:
- Letting your insurance know you have an appointment and reviewing your insurance coverage.
- Having a copy of your medical history ready.
Recent Research into Aortic Disease
Researchers in our Aortic Disease Program have published results in the medical journal Circulation. The study examined the genetic relationship in family members with in bicuspid aortic valve and thoracic aortic disease.







