What Is MicroTESE?
Microsurgical testicular sperm extraction (microTESE) is a surgical procedure used to retrieve sperm from inside a man’s testes (organs that produce sperm). It is an infertility treatment for men with non-obstructive azoospermia, a common cause of male infertility. Sperm retrieved during the procedure can be used for in vitro fertilization (IVF).
Our providers may recommend microTESE if you experience any of these conditions:
- You do not have ejaculated sperm, and there are no signs of blockage.
- You have an extremely low number of ejaculated sperm.
- You have tried other methods of sperm extraction that have failed.
MicroTESE Procedure: What to Expect?
For most patients, the worst part of microTESE is the idea of having surgery.
You’ll receive general anesthesia to help you sleep and stay comfortable during the procedure. When you’re asleep, your surgeon makes a small incision (cut) in the middle of your scrotum. The surgeon then opens your testicles and uses a high-powered surgical microscope to look for swollen seminiferous tubules (sperm-producing tubes). A swollen tube may contain sperm.
Next, your surgeon takes tissue samples from the tubes in one testicle. Your surgeon repeats this procedure on the other testicle. Finally, after collecting tissue samples from both testes, your surgeon closes the incisions with very fine stitches.
The surgeon gives the tissue samples to an andrology technologist, who examines them under a microscope. The technologist spends hours looking for sperm. If found, the technologist extracts the sperm and freezes it in liquid nitrogen. Then, you can use your frozen sperm for IVF (in vitro fertilization).
You may know immediately after surgery if there is sperm present. Sometimes you will be updated the day after surgery.
MicroTESE surgery risks may include:
- Bleeding
- Inability to find sperm
- General anesthesia risks
- Skin or testicle infections
- Transmission of a potential genetic cause of infertility to any offspring resulting from using the sperm
- Testicle damage
This is a modal window.
Find a Fertility Specialist
MicroTESE Recovery
Most men recover from microTESE quickly and have little pain after surgery. But your specialist may prescribe pain medication just in case.
Our surgeons use a specialized technique to close the incision that helps prevent infections and bleeding after the surgery. Additionally, the stitches dissolve on their own, leaving little to no scarring. The scrotum is one of the fastest-healing parts of the body.
Post-Surgery Care
Most patients find using an ice pack for 24 hours after the surgery helpful. For the first three days, take 800 milligrams of ibuprofen (Advil, Motrin) every eight hours and 650 milligrams of acetaminophen (Tylenol) every six hours to control pain and discomfort. If needed, take the pain relievers your provider prescribes.
You should avoid sex, masturbation, heavy lifting, or vigorous exercise for 10 days after surgery.
MicroTESE Success Rate
The microTESE success rate is favorable for most men. In fact, surgeons find sperm during approximately 40-60% of microTESE procedures. If you plan on using all of your sperm for in vitro fertilization (IVF), you may need more than one microTESE procedure.
While microTESE is successful for many men, surgeons don’t always find sperm during the procedure. If this happens and you choose to have microTESE again, the chances of your surgeon successfully finding sperm are very low.
MicroTESE Cost
Each microTESE procedure costs between $8,000–$12,000. So, it’s important to consider the testicular sperm extraction cost before deciding to undergo a second procedure. If microTESE isn’t a viable option, you can consider other ways to grow your family, including sperm donation and adoption.
Why Is MicroTESE Better Than a Biopsy?
We do not recommend fine needle aspiration or biopsy before microTESE for men with non-obstructive azoospermia. Studies show that microTESE yields the highest sperm retrieval rate and causes the least amount of damage to the testis.*
* Outcome of microdissection TESE compared with conventional TESE in non-obstructive azoospermia: a systematic review. Deruyver Y, Vanderschueren D, Van der Aa F. Andrology. 2014 Jan;2(1):20-4.
* Comparison of microdissection testicular sperm extraction, conventional testicular sperm extraction, and testicular sperm aspiration for nonobstructive azoospermia: a systematic review and meta-analysis. Bernie AM, Mata DA, Ramasamy R, Schlegel PN. Fertil Steril. 2015 Nov;104(5):1099-103.e1-3.
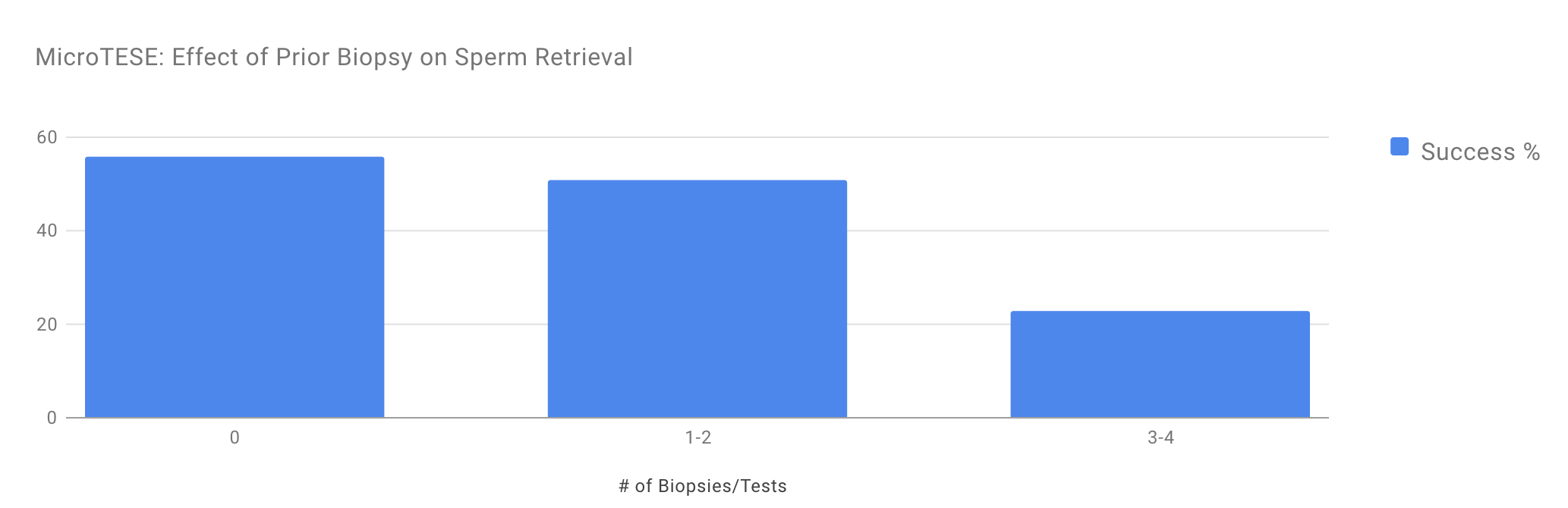
MicroTESE: Effect of Prior Biopsy on Sperm Retrieval
This chart shows why we don’t recommend performing mapping biopsies before microTESE. The graph in this figure shows the success of microTESE in men with non-obstructive azoospermia who have undergone 0, 1–2, or 3–4 prior testis biopsies attempting to find sperm. During microTESE procedures, doctors are able to find sperm in 56 percent of men who haven’t had a prior biopsy. Doctors find sperm in only 51 percent of men who’ve had 1–2 biopsies. For men who’ve had three to four biopsies, doctors find sperm in only 23 percent of men.
Put another way, if we performed a biopsy before microTESE and used it to determine whether or not to choose microTESE, we would not find sperm in half of the men where sperm could be obtained through microTESE.
MicroTESE vs. TESE (testicular sperm extraction)
Like microTESE, TESE (testicular sperm extraction) is a procedure that removes testicular tissue to look for sperm cells. But while microTESE helps if you have non-obstructive azoospermia, TESE treats men who have obstructive azoospermia. TESE is not right for men with non-obstructive azoospermia since it cannot look at all areas of the testicle to find those that produce sperm.
The TESE Procedure
During the TESE procedure your surgeon uses a small needle to numb your testicle and surrounding skin. Then, your surgeon makes a tiny incision (cut) inside your scrotum so they can extract a small amount of sperm from your testicle. Your surgeon cannot predict how much sperm they will find. But in many cases, one TESE procedure can fill several vials with sperm for later use. Alternatively, your provider may recommend a TESA (testicular sperm aspiration) procedure instead.
Surgery health risks such as bleeding, bruising, and skin or testicle infection can occur with the TESE procedure.
Your provider can perform TESE in their office while you are under moderate sedation or local anesthesia (which numbs a part of your body while you’re awake). You can also choose to have the TESE surgery in a hospital under general anesthesia (which puts you to sleep).
TESE After-Surgery Care
You should expect mild discomfort after TESE, but your provider may prescribe pain medication. Providers recommend taking 800 milligrams of ibuprofen every eight hours and 650 mg of acetaminophen (Tylenol) every six hours for the first three days. Avoid strenuous exercise and heavy lifting for one week, but sex and masturbation are OK after a few days.
Make an Appointment
Male infertility is a complex but treatable condition. The Utah Center for Reproductive Medicine offers medical and surgical solutions for many common male fertility problems. Our Andrology Lab is one of the only labs in the Mountain West to offer our wide range of common and advanced infertility testing procedures.
To learn more about microTESE, please call 801-587-1454 or schedule an appointment online. You do not need a referral from your primary care provider to make an appointment with our team.